5 min read
When Every Second Counts
How Metropolitan EMS and Baptist Health Medical Center worked together to achieve a remarkable outcome for one stroke patient When a woman in Little Rock, Arkansas, began showing signs of a severe...
The latest articles, case studies, research, and more are on their way to your inbox. Happy reading!

5 min read
How Metropolitan EMS and Baptist Health Medical Center worked together to achieve a remarkable outcome for one stroke patient When a woman in Little Rock, Arkansas, began showing signs of a severe...

4 min read
UCHealth Memorial Hospital is Using Pulsara to Facilitate Feedback, Education, and Better Outcomes Across Organizations What if the future of emergency care wasn’t just faster—but more united?...
1 min read
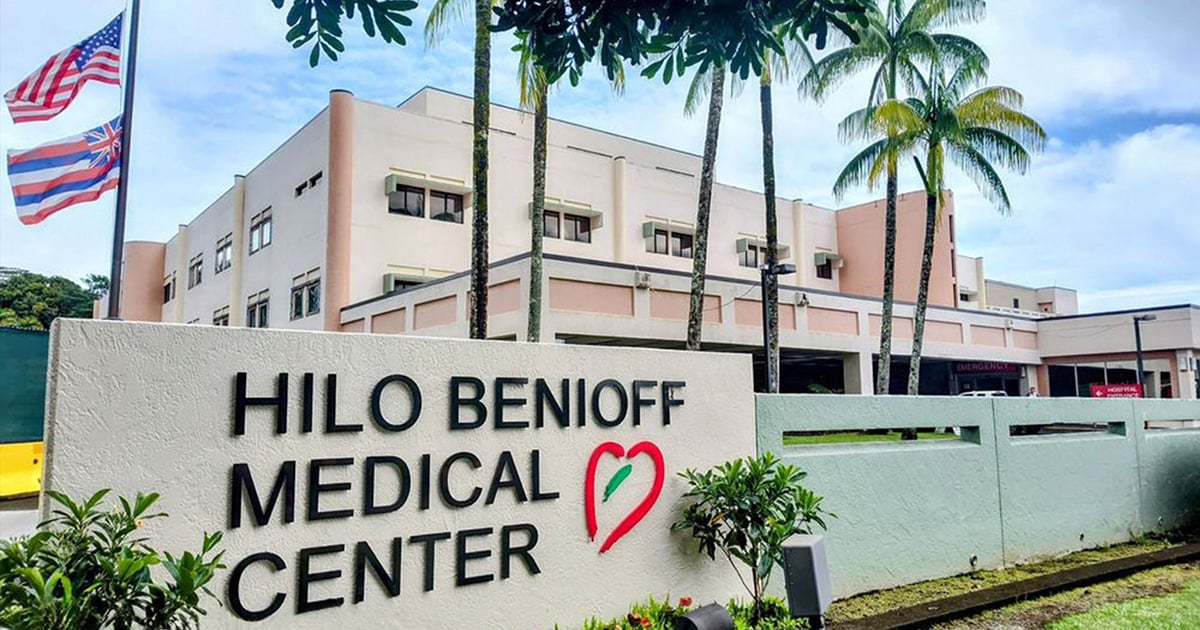
After implementing Pulsara, the Island of Hawaii's Hilo Benioff Medical Center achieved a 24-minute reduction in average door-to-needle time for stroke patients. Hilo Benioff Medical Center, the...

4 min read
Although they have the advantage of prior awareness and preparation, large-scale planned events pose unique challenges for emergency management teams. High patient volume, dispersed resources, and...

1 min read
A new study published by the AHA shows the use of AI and communication tools decreases treatment times between 43% and 53% for door-to-CT, door-to-needle, and door-to-puncture times A group of...

6 min read
EDITOR'S NOTE: This article originally appeared on FireRescue1.com. Special thanks to our guest author, Courtney Levin, for EMS1 BrandFocus Staff. Photo courtesy of Colorado Springs Fire Department:...

6 min read
Mass casualty incidents are among the most complex challenges faced by healthcare and emergency response systems. The stakes are high, and the processes can be overwhelming—from coordinating care...