Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
7 min read
 Team Pulsara
:
Aug 24, 2022
Team Pulsara
:
Aug 24, 2022

Editor's Note: On August 1st, 2022, EMS1, Fitch & Associates, and the National EMS Management Association released their fifth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is written by Kerri Hatt, Editor-in-Chief of EMS1.
EMS leaders respond to the 2022 EMS Trend Survey results with concrete steps to improve recruitment, retention, wellness, and safety
The EMS Trend Survey identifies where growth is needed to impact the sustainability and future of the industry. But growth requires a commitment to action.
We’ve asked a group of EMS veterans and up-and-coming leaders to identify areas where change is needed, as indicated by EMS Trend Survey results, and to offer action items for EMS supervisors, managers and chiefs.
By examining your service’s leadership strategies, and taking the steps outlined below, you’re on your way to elevating the safety, engagement and career health of your providers.
By Carly Alley, Executive Director for Riggs Ambulance Service
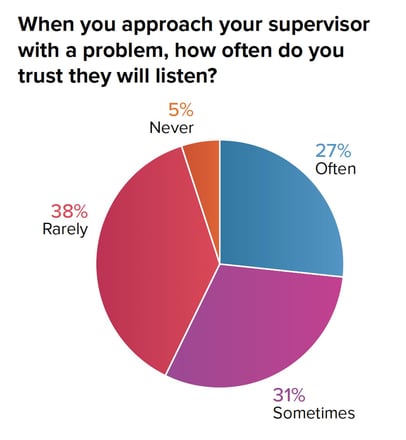
 In the EMS Trend Survey 2022, less than half of respondents felt their organization’s leadership is transparent. About 40% of respondents reported they rarely or never trust their supervisor to explain department decisions and, even worse, to listen to them when they approach leadership with a problem.
In the EMS Trend Survey 2022, less than half of respondents felt their organization’s leadership is transparent. About 40% of respondents reported they rarely or never trust their supervisor to explain department decisions and, even worse, to listen to them when they approach leadership with a problem.
As supervisors or managers, we often implement procedure/process changes that don’t make sense to our employees. While we see the whole decision-making process, our employees often are faced with the end result and simply expected to embrace the change. If we take the time to explain the “why’s” to our employees, it can make transitions to new processes easier, clear up any confusion as to why it was necessary to make the change, and provide direct support to employees during the transition.
It is imperative for us as leaders to gain input and feedback from our employees and use active listening skills when doing so. Our employees are on the front lines and have excellent insight into how our processes and procedures are working. When an employee brings up an idea or suggestion, take the time to sit down with them and discuss it. If at all possible, include employees in the planning process of a possible change or involve them in testing new equipment.
Although we can’t always fix every issue that is brought to us, we can provide feedback and loop closure to employees. By providing this type of feedback to our employees, we not only validate their concern/idea, we also provide them information about the organization they may not be aware of and help them understand why we were unable to make a change. This type of communication between management and employees builds trust and fosters a healthy relationship where employees feel comfortable sharing ideas and concerns and feels heard.
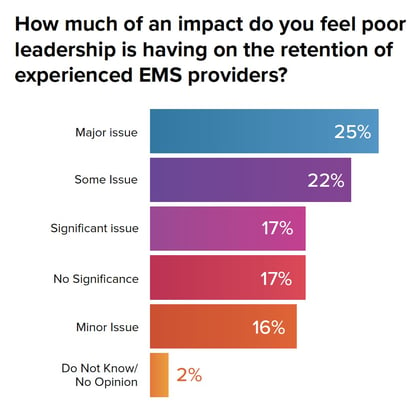
By Maria Beermann-Foat, PhD, MBA, NRP, Battalion Chief of Operations for MED-ACT- Emergency Medical Services, and course developer and instructor for the National Fire Academy Sixty-four percent of respondents have identified poor leadership as an issue worth paying attention to. As leadership quality is subjective, colored by respondents’ own unique lenses, we must first identify specific actions, traits or other factors that result in good or adequate leadership in order to address them.
Sixty-four percent of respondents have identified poor leadership as an issue worth paying attention to. As leadership quality is subjective, colored by respondents’ own unique lenses, we must first identify specific actions, traits or other factors that result in good or adequate leadership in order to address them.
We can start by looking at the open-ended responses to the question, “Please tell us what your direct supervisor does well and where they can improve,” where these predominate themes arose:
The emphasis on “soft” or “people skills” seems to support the adage that employees don’t quit jobs, they quit their bosses. Understanding this, today’s leaders should focus on professional self-development in these three focus areas. While we all like to believe that we’re decent communicators, the data does not support this for at least half of us.
Start by performing a self-assessment of your current communication style and practice. If your staff is willing to provide you feedback, that’s a great place to start to learn about where your communication is lacking. As is the case in most human-to-human interactions, there’s not a one-answer-fits-all communication style/practice. You will likely need to learn how to modify your communication style and practice to suit each member of your team. While this may seem overwhelming or impossible, the payoff for developing this skill can have the greatest impact. Ask each of your reports what they need to feel they’ve received “good” communication. You can also join a public speaking community (e.g. Toastmasters) to receive direct feedback from unbiased people. Reflect on how other people fail you in communication and take an honest inventory of where their performance and your own performance overlap.
If a supervisor has poor professional relationship skills, the ability of their team will be compromised and vice-versa. Professional relationship skills entail everything from how you treat people to how you make people feel when they interact with you, and impact your ability to make an employee feel cared for, appreciated and valued. This can be a difficult area to master which can be greatly hindered by department policies, organizational culture and operational practices. Improve your professional relationship skills by internal reflection (i.e. would you want to work for someone like you?), seeking one-on-one feedback loops and gathering anonymous performance data from your workforce.
The quickest, easiest way to start obtaining anonymous feedback is to send a mass email explaining your intent to professionally improve and then include a link to an anonymous online survey service (e.g. SurveyMonkey) with three simple questions to answer:
By Maia Dorsett, Emergency Medicine and EMS Physician at the University of Rochester Medical Center There were over 2,000 responses to the open-ended question asking respondents what their biggest safety concern was. Many responses centered around expected themes: vehicle safety, fatigue, violence against EMS clinicians. As I read through these responses, there were a few that stood out to me for the simplicity of their single-word response: “complacency.”
There were over 2,000 responses to the open-ended question asking respondents what their biggest safety concern was. Many responses centered around expected themes: vehicle safety, fatigue, violence against EMS clinicians. As I read through these responses, there were a few that stood out to me for the simplicity of their single-word response: “complacency.”
Merriam-Webster defines complacency as “self-satisfaction ... accompanied by unawareness of actual dangers or deficiencies,” perfectly summarizes the greatest threat to leadership’s ability to address key issues facing EMS clinicians. We cannot fix that which we are unaware of or do not understand. As clinicians, we cannot improve when we do not identify our weaknesses.
On the surface, we can name the threats we know: clinician burnout, turnover and the resultant workforce shortages. But awareness of deficiencies requires understanding the systems and ground-level issues that drive these threats. So how do we not only become aware, but engage frontline EMS clinicians in the solutions? We create environments where problems are openly discussed with candor so that individuals and leaders can work together to solve them – in short, psychological safety (something 2/3 of respondents felt was an issue within their organizations) becomes the norm.
Harvard Business School Professor, Amy Edmundson, writes that creating psychological safety in organizations begins with reframing the role of leadership from those with answers who give orders, to those who create conditions for continued learning. Reframing the role of EMS clinicians from subordinates within an organization to contributors with crucial insight begins with expressing gratitude when problems are brought up. Error disclosed? Gratitude. Problem identified? Gratitude. Solution proposed? Gratitude.
Complacency remains not just the greatest safety threat to our clinicians and our patients, but to the profession of EMS. While many of the larger problems will require significant national change, the daily wellbeing of EMS clinicians and the quality of clinical care rely on the development of local solutions through engagement of the frontline clinicians who do the essential and remarkable work of out-of-hospital medicine on a daily basis.
By Rob Lawrence, Director of Strategic Implementation for PRO EMS and part-time Executive Director of the California Ambulance Association
 The training of our supervisors always gives me cause for some concern as there is the perception that because they are good medics, they automatically make good supervisors. Sometimes, this isn’t the case. I am a firm believer in the Peter Principal, the notion that we promote good people to a level of incompetence, and this is through no fault of their own. We must make sure we train and educate those we promote to be equipped and prepared for the new position. Some of the comments in the EMS Trend Survey responses reflect this notion. It isn’t the supervisor that needs to improve; in many cases, it is the organization employing them. Leadership training must occur to both inspire and prepare those for greater responsibility.
The training of our supervisors always gives me cause for some concern as there is the perception that because they are good medics, they automatically make good supervisors. Sometimes, this isn’t the case. I am a firm believer in the Peter Principal, the notion that we promote good people to a level of incompetence, and this is through no fault of their own. We must make sure we train and educate those we promote to be equipped and prepared for the new position. Some of the comments in the EMS Trend Survey responses reflect this notion. It isn’t the supervisor that needs to improve; in many cases, it is the organization employing them. Leadership training must occur to both inspire and prepare those for greater responsibility.
By Casey Patrick, MD, FAEMS, Medical Director for Harris County ESD11 Mobile Healthcare and Assistant Medical Director for the Montgomery County Hospital District EMS Service
 One central theme from the EMS1.com 2022 EMS Trend Survey was a significant amount of concern from medics regarding safety related to appropriate call deployment. EMS foundations have definitely been shifting as mounting evidence questioning the effectiveness and necessity of ambulance response and transport utilizing red lights and sirens (RLS) has progressed.
One central theme from the EMS1.com 2022 EMS Trend Survey was a significant amount of concern from medics regarding safety related to appropriate call deployment. EMS foundations have definitely been shifting as mounting evidence questioning the effectiveness and necessity of ambulance response and transport utilizing red lights and sirens (RLS) has progressed.
While current data does indeed suggest minimal time savings and rare life-saving intervention necessity in conjunction with red lights and siren use, EMS professionals cannot dictate response decisions based entirely on “the literature” alone.
All community, hospital and public safety stakeholders should be involved and educated throughout the decision-making implementation of RLS reduction tactics. Finally, local data is key to establishing concrete and relatable reasoning from a community, medic and patient safety standpoint. With evidence in our corner, RLS reduction should be an EMS goal for the present. However, resistance will likely be overwhelming without cultivated partnerships and a true community story.
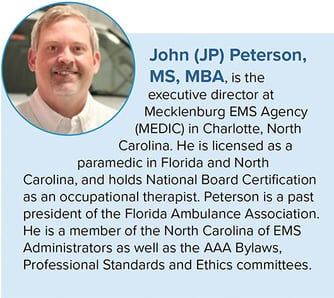
By John (JP) Peterson, MS, MBA, Executive Director at Mecklenburg EMS Agency
 In the open-ended EMS Trend Survey question, “Why would you recommend or not recommend EMS as a career,” one of the commenters noted, “It is the last of the great healthcare apprenticeships. The scope of work and rewards is beyond other professions.”
In the open-ended EMS Trend Survey question, “Why would you recommend or not recommend EMS as a career,” one of the commenters noted, “It is the last of the great healthcare apprenticeships. The scope of work and rewards is beyond other professions.”
I have heard EMS described as a “stepping stone” to other healthcare or public service careers. Oftentimes, this is due to a feeling of limited upward mobility in an organization or a desire for better pay, benefits or work schedule. I started my career as an EMT and eventually worked my way up the ranks to become a chief operating officer and executive director. This career path was possible because my organization created a clear advancement pathway and worked with me to be successful. They were supportive of me even when I was in school for a non-EMS degree. That support and guidance led to me to ultimately decide to make EMS my long-term career.

An EMS organization that is investing in its employees and promoting longevity in the profession is one that makes the effort to elevate people to be successful, assisting them to identify what success looks like and how to achieve it, as well as supporting them in their dreams and aspirations. If EMS professionals believe that they will have opportunities to grow within an organization, pay and benefits that allow them to thrive, and know that their employer is invested in their success, there is a good chance that they will see a future in EMS.
Download the full 2022 EMS Trend Report
About the author
Kerri Hatt is editor-in-chief, EMS1. She has a bachelor’s degree from Saint Joseph’s University, in Philadelphia. She is based out of Charleston, SC. Share your personal and agency successes, strategies and stories with Kerri at khatt@lexipol.com.
After two years, the pandemic is still impacting every aspect of the EMS profession – from recruitment and retention, to safety, to how you assess and treat patients. See the 2022 EMS Trend Survey results.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...