Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Editor's Update: The ET3 program is mentioned in the report below. Please note that, as reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
Editor's Note: On August 1st, 2022, EMS1, Fitch & Associates, and the National EMS Management Association released their fifth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is written by Anthony W. Minge, EdD, senior partner at Fitch & Associates.
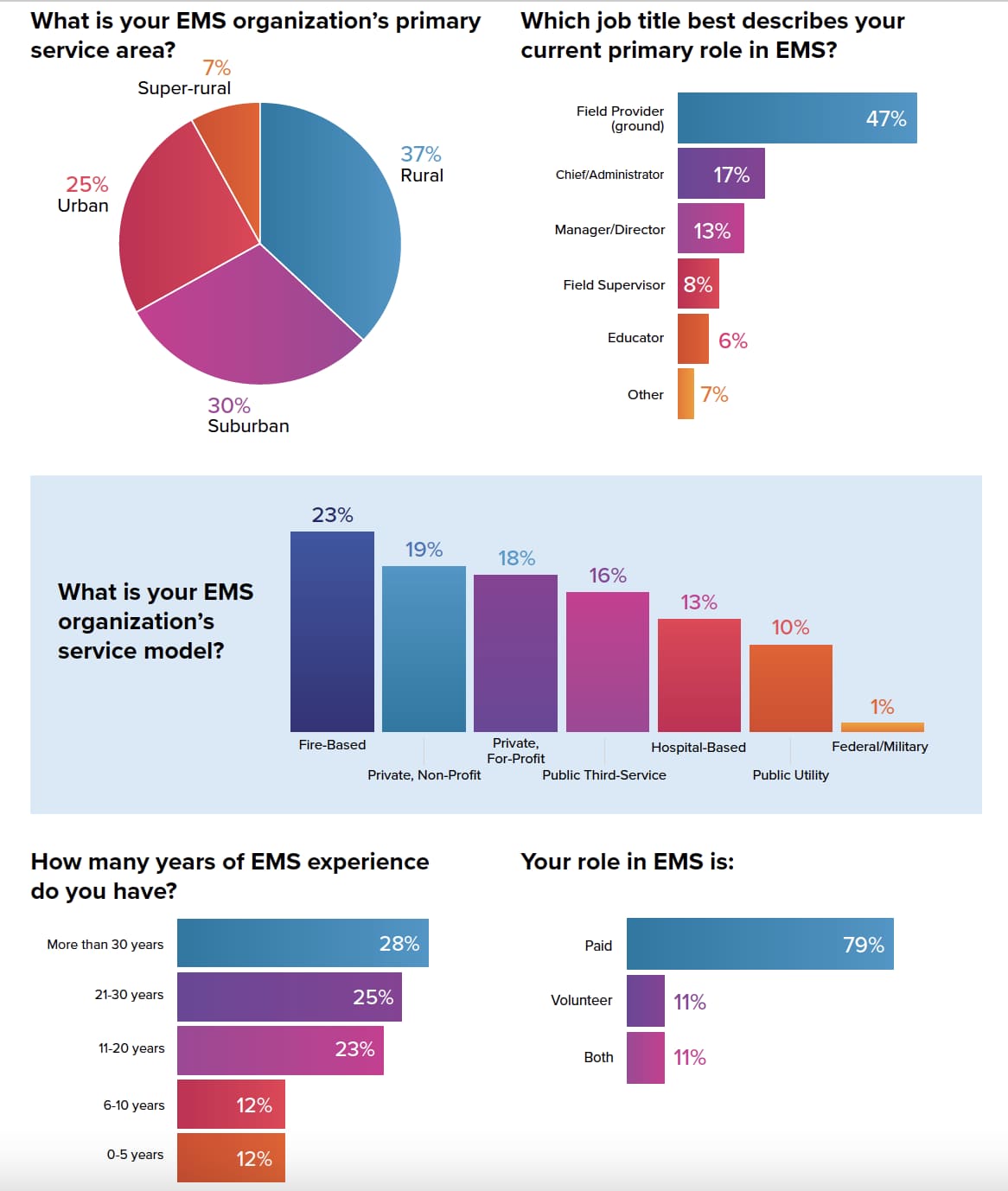
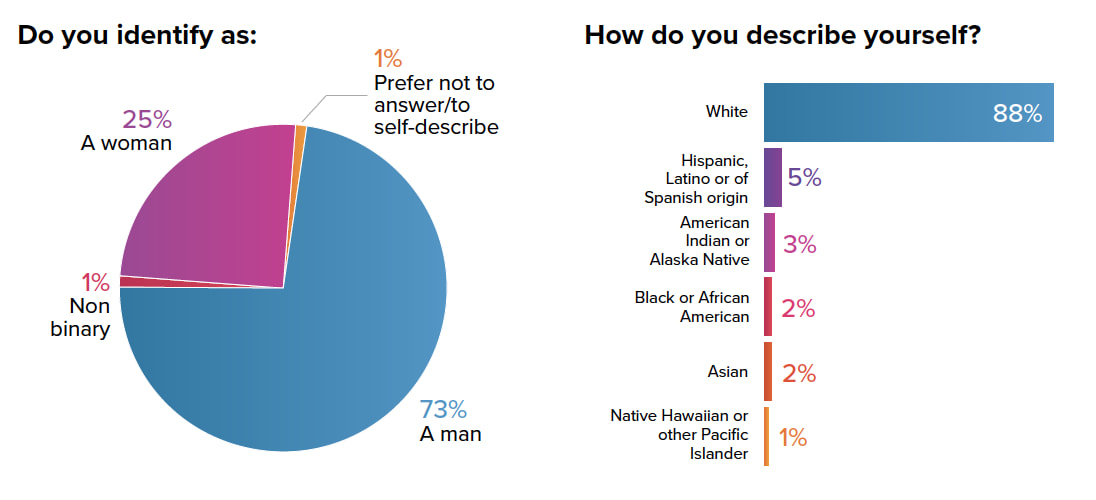
Survey questions for the EMS Trend Survey were developed through a collaboration between EMS1, Fitch & Associates and the EMS Survey Team – which was instrumental in collection and interpretation of data. The EMS Trend Survey was conducted online in early 2022. The survey was widely promoted and open to any member of the EMS community. More than 3,200 people responded, the most in the survey’s history. They represent a wide range of service models, certification levels and years of experience, and every region of the nation.
The 2022 EMS Trend Survey results reinforce what many of us see every day. More than two years into the pandemic, it’s still impacting every aspect of our profession – from recruitment and retention, to safety, to how you assess and treat patients.
As we have realized that this pandemic is not just a flash in the pan, but something we may be dealing with for a long time, we have also been able to move forward. Many innovations that departments initially put on hold because of COVID-19 have now been implemented. In other cases, changes wrought by this global health emergency now have uses well beyond COVID patients and may be with us, helping patients and the people who care for them, for years to come.
Clearly, the pandemic has halted progress in some areas – and taken a toll on our organizations and personnel – while also providing an opening for new technologies and ideas to revolutionize healthcare, including EMS.
This year’s EMS Trend Survey, our seventh annual survey of EMS clinicians and leaders, reflects these realities. We continue to have divisions within our ranks, but are also unified in many areas.
While our profession has many challenges before us, we know exactly what they are, and in some cases, even how we can try to address them. But it will take true leadership – yes, from the people whose titles and rank give them authority, but also from the leaders within every level of every organization – to move past those obstacles and transform the profession into what we know it’s capable of becoming.
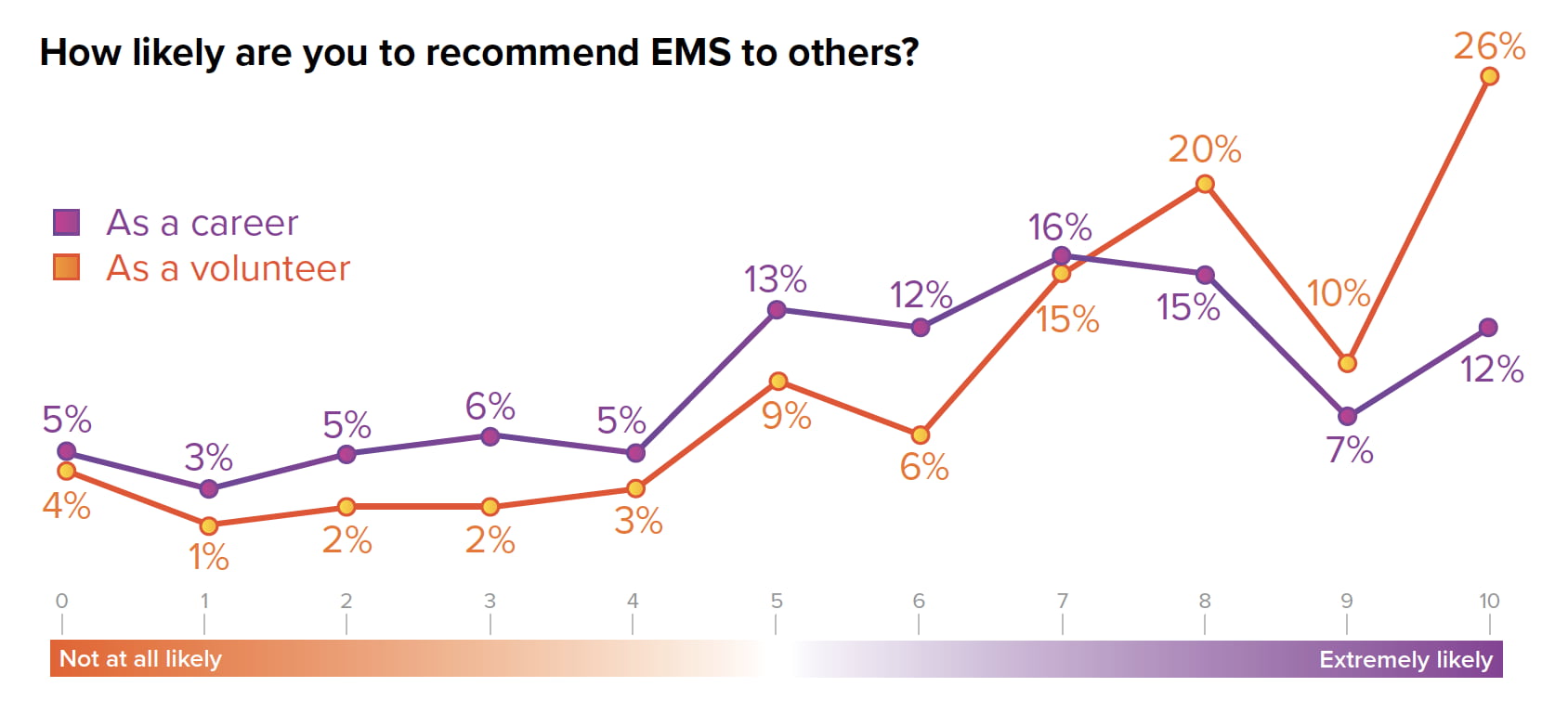
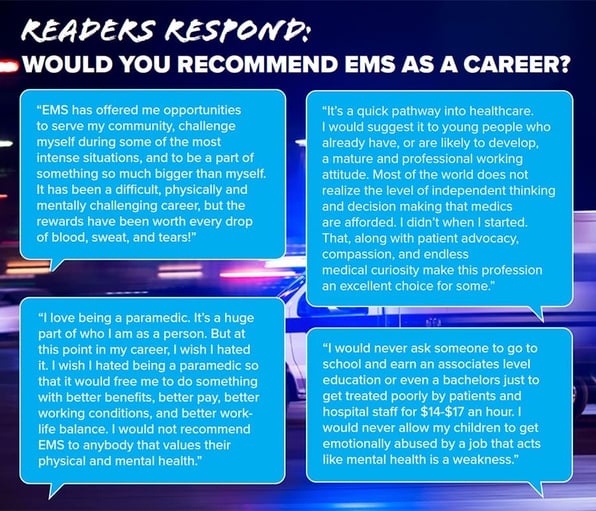
Despite two years of a pandemic, piled on top of decades of underfunding and poor pay, many of those surveyed would still recommend EMS to others. More than half of career EMS professionals reported they were likely to tell others to pursue EMS as a career, while over 70% of volunteers reported they would recommend volunteering in EMS.
While this might not seem that promising – on a scale of 1-10, with 10 being the most likely to recommend EMS as a career, only 50% chose seven or higher – it’s actually relatively positive compared to many other public safety or healthcare professions. For example, in the 2022 Police1 State of the Industry survey, only 22% of respondents chose 7 or higher (out of 10) when asked how likely they were to recommend a career in law enforcement. And in a 2018 survey of more than 3,000 physicians – that’s right, even before the pandemic – only 26% of doctors said they would recommend medicine as a career to their own children.
Similarly, when we compare this year’s responses to those from 2 years ago – when the survey was conducted prior to most of us knowing what COVID-19 was and before any shutdowns – EMS clinicians and leaders’ optimism hasn’t diminished. In 2020, when presented with the statement, “I am optimistic about the future of EMS,” 42% said they agreed, 38% disagreed and 19% were neutral. This year’s survey shows a slight shift toward optimism compared to two years ago, with 50% agreeing with the statement and only 31% disagreeing.
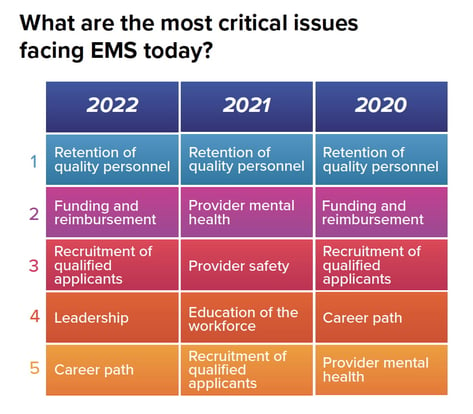
Interestingly, 2022 looks like 2020 again in other ways as well – almost as if the pandemic didn’t happen. In 2020, respondents identified the top three concerns facing EMS as, respectively:
1. Retention of quality personnel
2. Funding and reimbursement
3. Recruitment of qualified applicants
Then, in 2021, after a nearly full year of COVID had turned the world upside down, things shifted. While retention remained No.1, provider mental health and provider safety vaulted from fifth and sixth on the list to second and third. This year, they’ve dropped again, with the top three looking identical to two years ago, pre-pandemic.
That said, clinician mental health remains a concern. When asked specifically about different safety concerns, including physical safety, vehicle safety, psychological safety (ability to speak freely without reprisal), violence against caregivers and mental health, respondents broadly reported that the latter three were more of a concern than vehicle and physical safety related to their jobs. Nearly 80% said that mental health was an issue they were concerned about.
And while nearly a third of survey respondents said they have no symptoms of burnout, that means the majority – 60% – reported having at least one symptom, while 9% reported feeling completely burnt out.
Are agencies doing anything to address this problem? The answer is clearly yes and no. When asked about their organization’s employee assistance program, 26% agreed that EAP staff understands the work of EMS providers, while 38% disagreed. Just over one-third of respondents said their agency has an effective peer support program (outside of EAP), while an almost equal number said their agency does not.
When asked what leadership behaviors or actions mattered most, four words blew away other responses:
Overall, 49% of respondents felt their organization’s leadership is transparent, while 34% disagreed and 16% were somewhere in the middle.
We specifically asked people who identified as either flight or ground field providers or field supervisors about their interactions with management. What we found was encouraging in some areas – 80% said they have one-on-one meetings with their supervisors sometimes or often – but left room for improvement in others:
Overall, respondents working in the field felt their supervisors allowed them the freedom to do their jobs, and more than half said their supervisors help them learn from mistakes – which aligns with another question, in which 58% of all survey respondents agreed that their organizations approach safety concerns or mistakes as opportunities to grow, rather than chances to place blame.
In open-ended questions, field providers said they want leaders and supervisors who listen, are transparent, and who express empathy and compassion. It’s clear expectations of leaders are changing, and EMS clinicians know that leadership training and education are as critical as clinical education.
When asked what their supervisor could do to improve, one respondent wrote, “Focus on building EQ and listening skills. In my former corporate executive world, I would have sent my current EMS supervisor to multiple management development classes and if they continued to operate the way they currently do, I would have reassigned them or managed them out of the organization.”
Another common theme was communication. “Periodically, I feel that my direct supervisors sometimes think that we know more than we do about operational changes so communications tend to fail,” one person wrote.
While the EMS Trend Survey helps us get a sense of what people think across the country, it doesn’t tell you about your own agency. Do you know how your employees feel about your leadership? Or how it’s impacting patient care?
Our results show that many organizations might be missing opportunities to gather critical information. Only 34% of respondents said their organizations conduct employee engagement surveys, which are a valuable way of measuring trends and evaluating your organization’s health. Similarly, a third of respondents said their agencies currently conduct patient experience surveys, and only a handful reported plans to start doing so soon. If we don’t regularly survey people in a systematic, validated way, then we don’t really know how our system is performing in those areas – we’re just guessing.
The majority of survey respondents continue to say their organizations struggle to recruit qualified EMS clinicians. With recruitment and retention still identified as top challenges facing the profession, this year we looked deeper at some of the reasons, focusing on retention – which many organizations have recognized as an area often neglected in favor of more expensive recruitment programs, including signing bonuses.
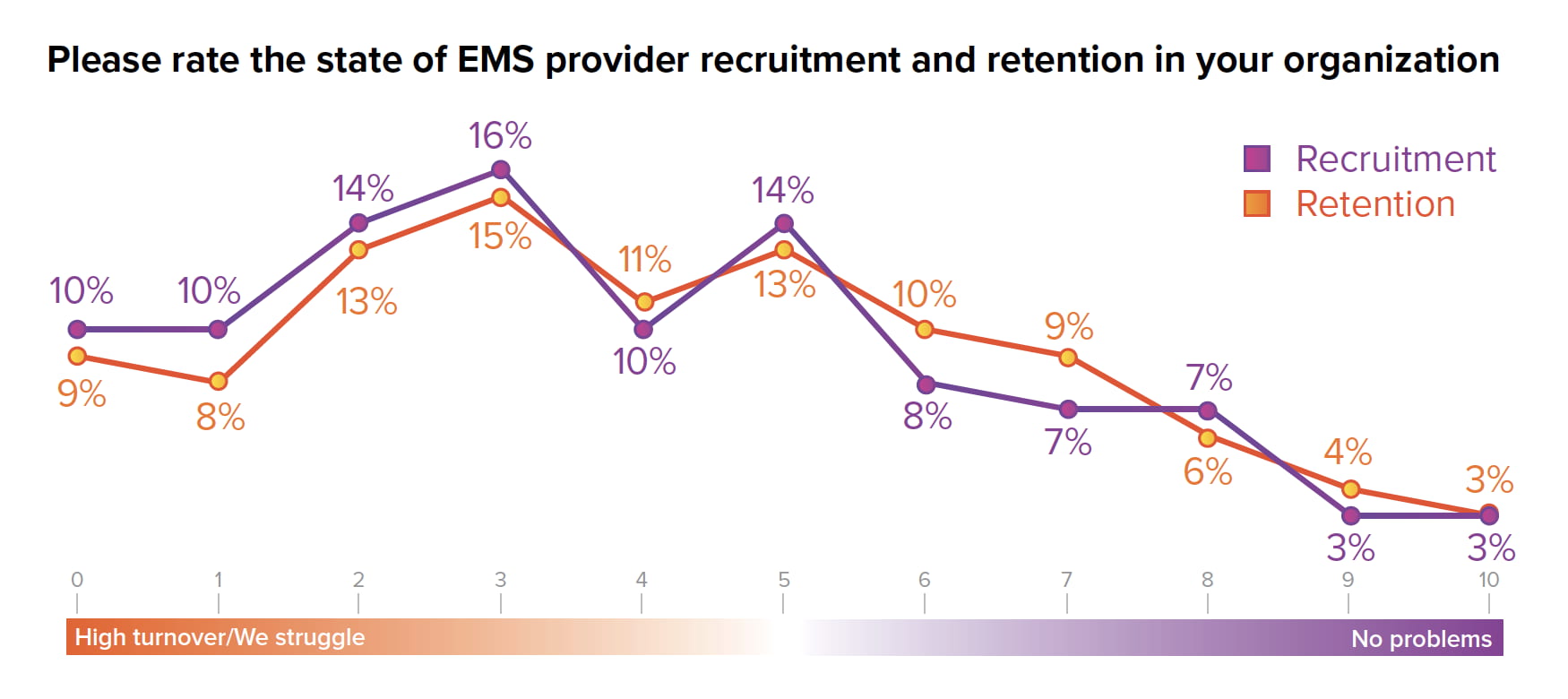
Respondents were asked how much of an issue several factors were when it comes to the retention of experienced EMS clinicians. Here’s what we found:
While the majority of survey respondents said they had no plans to leave their current employer, many still do, in numbers similar to 2020 and 2021. One slight difference, however, is an increase in how many say they plan to pursue careers outside of EMS or even outside of healthcare entirely, with 19% saying they’ll move on to another healthcare job and 17% saying they hoped to leave public safety and healthcare entirely.
While this year’s survey focused on the state of the profession and attitudes of EMS clinicians and leaders, we continued to ask some questions related to operational and clinical trends. Although the use of telehealth skyrocketed during the pandemic and remains much higher than pre-COVID, its adoption within EMS remains relatively low, with only 18% of respondents saying their agencies are using the technology to connect patients to physicians or other providers.
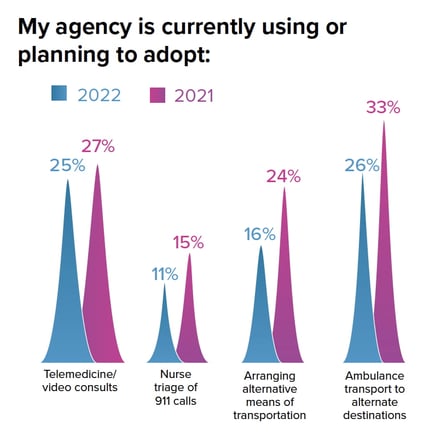
Similarly, there was no substantial change in the use of nurse triage of 911 calls, arranging alternative means of transportation for patients, or transporting to alternative destinations. It’s only been a little over a year since the Center for Medicare & Medicaid Innovation kicked off the Emergency Triage, Transport & Treatment (ET3) model, a five-year pilot program allowing nearly 200 EMS agencies to get reimbursed by Medicare for these alternative programs. It’s too early to tell what the results will be, with some organizations reporting early success and others the opposite, but it’s clear that some of the momentum behind such programs has stalled, possibly as EMS leaders wait to see if CMS or other payers actually make any significant policy shifts.
Also of note:
So, what does it all mean? Well, for one thing, EMS clinicians are looking for leadership. But they’re also looking for good management. In other words, we need to truly foster the next generation of leaders who can inspire people to excel – by listening, by communicating, by promoting transparency – and by creating and articulating a shared vision that inspires the workforce.
Last year, I admit, I was a little naive. In the 2021 EMS Trend Report, I wrote the results showed that while the pandemic had tested the profession, it had not crippled us: “the real test will come next year, once we’ve had more time to recover and, perhaps, reinvigorate our efforts to improve,” I wrote. Of course, we all realize now that the time to “recover and reinvigorate” is not going to come easy.
In EMS, there will be no breaks, no time to sit back and reflect on the past and create our future. Unless, of course, we decide together that we have no other choice. The 2022 EMS Trend Survey doesn’t hold all the answers, but I hope it inspires you to start asking the questions – within your state, your organization, even yourself. Then, commit to creating the next generation of leaders – or to becoming part of that generation.
Because it will take true leadership to tackle these issues, to show political leaders and the public that an investment in EMS is an investment in communities, and to create a brighter future for EMS clinicians everywhere.
Download the full 2022 EMS Trend Report
About the Author
Anthony Minge, EdD, is a senior partner at Fitch & Associates. He has more than two decades of leadership, revenue cycle management, compliance and healthcare business operations experience. Prior to joining the firm, he was the business manager for Northwest MedStar in Spokane, Washington.
Telemedicine, community paramedicine, and mobile integrated health programs are changing the face of EMS. Here are 10 things you need to know.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...