Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
5 min read
 Team Pulsara
:
Sep 15, 2021
Team Pulsara
:
Sep 15, 2021
Editor's Update: The ET3 program is mentioned in the below article. Please note that, as reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
Editor's Note: This article originally appeared on EMS1.com as "Medical Direction: Stepping Up the Ladder." Special thanks to our guest author, Casey Patrick, MD, FAEMS, Assistant Medical Director for Montgomery County Hospital District EMS.
__
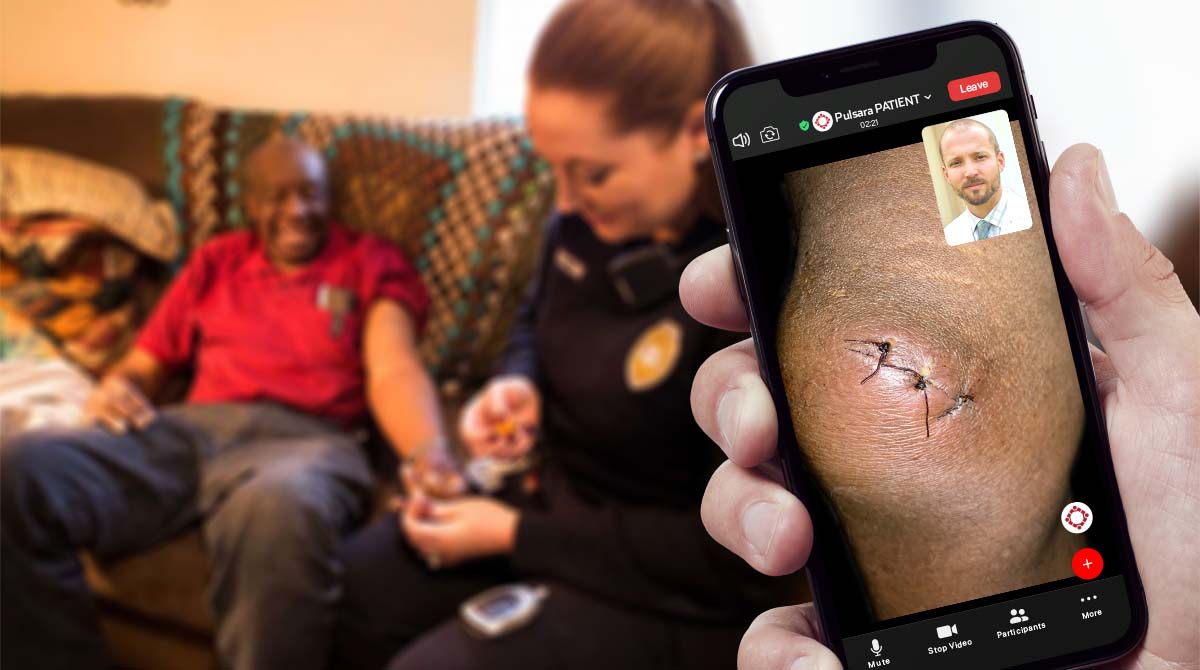
MCHD has been using mobile communication technology to allow medics to consult their medical directors, sharing audio, snapshots, and video from inside the patient's home or the ambulance
At Montgomery County Hospital District EMS service in Greater Houston, we looked for a streamlined way to step critically ill patient prehospital care up the ladder to medical direction.
Our telehealth journey began when we integrated the Pulsara communication app about two years ago, both as our intra-service communication tool and with a vision to progress to use it with our receiving hospitals.
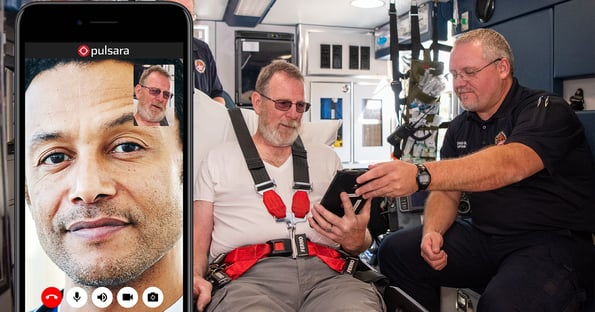
Real-time communication allows the medics to consult a district chief, a supervisor, a high-ranking medic—or, as in our case—a medical director, sharing audio, snapshots, and video from inside the home or the ambulance.

Sometimes, the medics will just call to report a voice memo clip. Often, the crew will attach pictures (e.g., if they're in a nursing home, they may send a past medical history or a medication list). I'll get a snapshot with the EtC02, the rhythm on the monitor, or the length of time the monitor has been on, which is incredibly helpful.
We recently purchased the portable Butterfly iQ+ ultrasound product. The on-scene medics can upload the ultrasound images and elevate them for medical direction to review in real-time.
I have had a handful of cases since we've implemented where the medics will call and say, "Hey, we started in what we thought was PEA, but after a couple of rounds of drugs and fluids, I think we have squeeze (cardiac activity). Can you take a look?" Then I'll review the images; "Yes, I see clear cardiac motion; that one warrants fluids and vasopressors."
The medics can also type in a brief summary, so you can get a whole picture of the resuscitation and what's been done. It makes it very easy to see patient status and what is available to the entire team simultaneously, as opposed to the old school radio or phone call, where it's just verbal, and you're relying on a good connection.
We now have Wi-Fi connections and Wi-Fi hotspots in the truck, which allows for more visual input, both of the monitor and the patient's history. When you add in ultrasound and the patient's history. When you add in ultrasound capability, the actual four chambers of the heart are visible as well.
Telehealth connection offers a complete picture of what's going on, and you're less dependent on a signal and a quiet spot, which we all know, in the world of EMS, you don't always have. It is just more consistent from a communication standpoint.
For smartphone users, the training process for implementing this type of application is relatively minimal. Realistically, if you can use iMessage, WhatsApp, or text on your phone, it's reasonably intuitive. At MCHD, we rotated all the medics through a brief training session, and let them run through mock cases.
We gave our medics the option of using and downloading the app on their personal device or downloading it on the company device. [Ultimately], we equipped each truck with two iPads. Other than this upfront expense of providing each medic a device for their shift, the costs involved in this type of telehealth platform are relatively negligible when considering the error reduction potential and ability to streamline overall communication.
If your partner hospitals decide to use communication application's time-sensitive emergency packages to pre-alert on down the chain, that's where the cost comes into the hospital. But the benefits—reduced errors, decreased triage time, and improved turnaround times—are beneficial to both parties.
Realistically, half the time in the ED, when staff is receiving those radio calls from incoming EMS units, they're working 16 other things at once in a noisy environment. A patient might be coding next door, with monitors going off in the background; it's impossible not to miss details.
Why are we radioing? Radio reports are often too long and provide information overload. Our thought process was, "how do we communicate normally?" We communicate with text, and we communicate with our smartphones and our smart devices.
When the report comes in via text, you don't have to hear over the ambulance and the ED's background noise. If you didn't catch it the first time, the report is saved on the device. It's more error-resistant.
We partnered with the Memorial Hermann system here in our county to bring text reporting on board, and we're using it for both general medical reports and stroke activations.
As the medic, if I'm bringing in a patient with abdominal pain, I'm going to snap a picture of the monitor, med list, and insurance card/ID. The hospital has all the information to pre-register the patient based on a single information share, which probably takes less time than a radio call would. The ED then can track the arriving unit via GPS, so it's not, "I'll be there in five minutes," which, in reality, means, "I'm pulling in the driveway." Everyone knows precisely when the EMS truck is arriving.
It just makes sense to take those things that generally happened while standing in the triage bay and allow them to occur in parallel pre-arrival. Converting linear processes to parallel moves things even further towards the front, saving time and getting units back into service quicker.
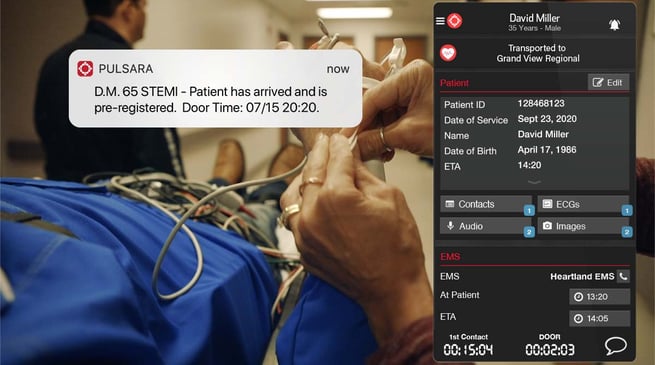
Early evidence suggests that prehospital stroke team activation decreases turnaround times at the hospital. We aim to track our data and expect to see the same within the MCHD system. Over time, we will be able to look at door-to-needle time, door-to-CTA time, door-to-TPA time, etc., to see how earlier EMS notification in a more formal fashion affects not only ED care, but also the neurologist, and the neuro-interventionalist and intensivist.
Depending on how your system's online medical control works, whether it's medical supervisor or medical supervisor to medical director, the flexibility exists for any sized system. You can program who is on each team, cardiac arrest, STEMI, or stroke. It's straightforward to turn alerts on and off for different folks within each string. For example, I don't get alerts for all incoming patients to the hospital, but I am on alert for critically ill patients.
It's a learning process. Old habits are hard to break. Sometimes, people revert and pick up the radio and call. But so far, everyone's pleased. Ideally, the rest of the county's receiving hospitals will adopt the same platform, which will lead to proper regionalization. Our system goal is to move away from one practice for hospital A and another practice for hospital B.
Though MCHD is an ET3 participant, COVID-19—and the bandwidth it has occupied, with a county-wide spike, and the impact on staffing with quarantined and infected employees—has delayed implementation here until the start of 2022.
Some larger EMS systems have just recently gone live with their ET3 programs. As a more mid-size service, we are hoping to learn from their experience. Mutual collaboration will be essential moving forward.
We foresee a role for telemedicine in the ET3 program, both within our treat-in-place protocols and in our alternative destination plan as well. While telehealth medical direction will allow us to toggle between these two pathways, we still have many implementation hurdles to cross. Billing, coding, and documentation are all in development from scratch, with no exact blueprint. Especially with the COVID-19 pandemic and the associated drop in transport volume, we have to be very sensitive to any significant changes affecting overall budgets and payment structures.
We'll be looking to the systems implementing ET3 in the next few months and the proof of concept that's occurring to identify the sticking points and how we can streamline our implementation.
About the Author
Dr. Casey Patrick is the assistant medical director for the Montgomery County Hospital District EMS service in Greater Houston where he helped develop and currently produces the MCHD Paramedic Podcast. Dr. Patrick is board certified in both Emergency and EMS Medicine and works as a community emergency physician in multiple states. Additionally, he is an active member of the Texas NAEMSP State chapter and the national association, and serves as an EMS1 Editorial Advisory Board member.
To learn more about how hospitals and EMS organizations are using Pulsara, check out our customer success stories. Pulsara is also helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...