Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
16 min read
 Team Pulsara
:
Nov 17, 2022
Team Pulsara
:
Nov 17, 2022

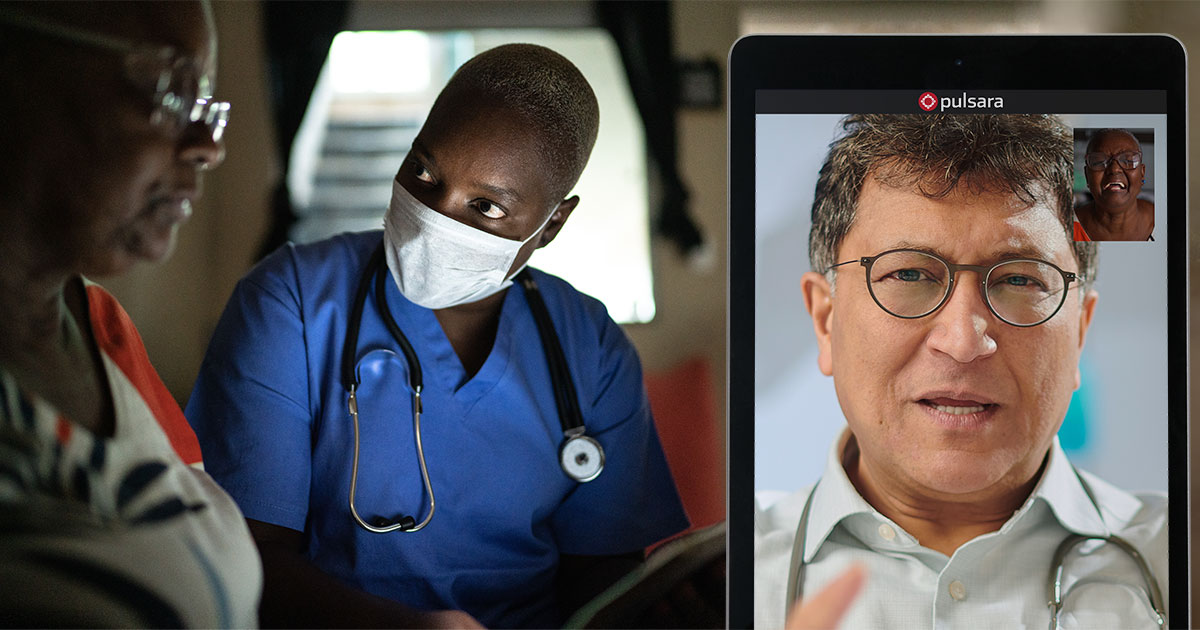
Prior to the COVID-19 pandemic, Teller County, Colorado, had a successful community paramedicine program in place. But as the pandemic hit the U.S., they knew they'd need to leverage new tools to continue treating their patients. Fire and EMS leaders partnered with Pulsara to enhance their community paramedicine program with telehealth. Since then, the program has evolved into a thriving partnership between EMS and a local organization of board-certified emergency physicians, allowing them to work together via telehealth to help address healthcare disparities and improve access to care in rural areas.
In a recent webinar, Dr. Jeremy DeWall, EMS Medical Director at UCHealth Pike's Peak Regional Hospital, and James McLaughlin, Director of Community Paramedicine at Ute Pass Regional Health Service District, shared their experience with building the program, and how they are using telehealth as a force multiplier to preserve EMS resources while also better meeting the needs of their community.
Watch the full webinar below, or read on for part 1 of our webinar coverage.
Q: Dr. DeWall, you’ve been working in this area for around 12 years, and James, you for around 14 years. You both recognized the need for something better. What were some of the biggest challenges you faced that led you to set up a new way of doing things—particularly, employing a telehealth system?
James McLaughlin:
The region that we serve is a very mountainous area, and it tends to be extremely geographically isolated. We have large populations that have been marginalized because of their inability to access care. We have patients who need primary care, patients who need behavioral health services, and patients who need specialty care. They really struggle with accessing that care, because there are just not enough providers to provide care in those areas. And then the other problem is, people have a hard time getting rides, especially when we start talking about our marginalized populations, like our elderly populations, who don't drive.
Our average lot size for somebody who owns or rents a residency in our area is about five acres. A lot of these folks tend to live in those areas for a reason. Obviously, we're generalizing here, but a lot of them don't have a very robust social support system to help guide them and provide them with services. We had established this program initially to address some of those disparities.
And then COVID-19 kicked off, and we really started to see an increase in fear across the country. In our community, we saw people that were just terrified to go to the hospital. We saw people that were literally dying because they were afraid to access the care that they needed. And honestly, a lot of people couldn't access care with their primary care providers. So that need for care would go unmet.
And we even saw in our area (as I think we did across the country) the number of people calling 911 significantly decrease. That was a major concern for us. We wanted to keep our providers safe, but also increase the value that we provide to the service and to the community.
We had this program. We were starting to use it in other areas. And we got together and decided that this was the tool that would help us increase the services that we provide to patients.
So we partnered with Pulsara to develop an enhancement to their platform that allowed us to send a link to a patient before we ever arrived on-scene and actually start that communication process before we ever made contact with the patient. And then once we made contact with the patient, we were able to then link with our primary care providers and the groups that we work with, so that the patient could have direct access to care through that network.

Q: What is this telehealth system all about, and why did you choose it over utilizing existing communication methods, such as faxes, radios, and pagers?
Dr. Jeremy DeWall:
When we were looking at this in COVID-19, as James mentioned, the issue was a bit about COVID, but it melded very quickly into patients being afraid to just go to an emergency department because they were worried they were going to contract COVID-19. As James mentioned, [they were] fearful of actually accessing the health care system. Or, quite frankly, not being able to access it. Because if you had a cough, a cold, or a sore toe, you were essentially told by the primary care physicians: ‘We can't see you, because we can't risk getting COVID ourselves.’ It really restricted access to our patients.
When we look at our telehealth data, about 14% of patients in our area don't have a primary care physician. Which means 86% of our patients do have a primary care physician, and yet we still see utilization of telehealth, probably because they can't get into their local primary care physician. And that's a problem in urban areas as well as rural and frontier areas. I think throughout the United States, there's a lack of ability to get in, even if you have a primary care doc.
So what we looked at with this was: how can we get a physician working with community paramedics and/or other EMS providers directly to the patient?
And honestly, when we started out in COVID, we had no idea what to use. We looked at multiple platforms. We even looked at WhatsApp, because we did have some state allowances and waivers to be able to utilize systems that otherwise would not be allowed, in order to try to access patients in the middle of the COVID-19 pandemic. Obviously, we decided that was probably not the best choice, and really tried to pursue something that would work.
The reason we ended up settling with Pulsara is, quite frankly, it's known to EMS. Within our region collectively, all of our EMS services have used Pulsara for numerous years to improve our STEMI care, stroke care, and hospital communications.
So when we started looking at other platforms and trying to figure out what would work, we found that something that EMS consistently used in daily operations was likely to work best in these new environments and in the middle of a pandemic, when providers were burnt out. And as our providers have said, ‘We never spent so much time learning stuff to not respond to calls.’ We really looked at that and said, ‘How can we best roll something out without burning out our EMS clinicians?’
Now, when we looked at Pulsara, they didn't actually have the ability to do [video telehealth] yet. We approached them because we were using them for other things and said, ‘We have a goofy idea. We need video telehealth, and we need it today.’
And within a month, they came back to us with the telehealth capabilities we needed. Ute Pass Regional Health Service District was the original spot, and as we talked about, we've expanded to other agencies, and will likely be expanding further in the future.
Q: How did your patients feel about this new telehealth program? Was there much resistance, or did they embrace it?
James McLaughlin:
I love this question, because I was very concerned at first. We do have a large population that's geriatric. We have a large population that's anti-technology. And I really was concerned that there was going to be some pushback on adopting this product. And I think there would have been if it hadn't just instantly worked so effectively and so well.
I’ll be honest, I was an initial naysayer of the technology. I wasn't convinced that this was going to be the answer for our needs. I was probably one of the loudest people against adopting the Pulsara technology. I felt that it was going to increase the workload for our providers and put a lot of extra work on them.
And what I've been absolutely mesmerized by is the fact that it just works. The user interface works exactly like you would expect it to. Every button does exactly what you would expect it to, and that's what our end users see as well.

So when our providers are out there, especially early on when we first adopted the telehealth process, they have a lot of new skills and abilities that they're implementing. And what's great about this is it doesn't task-saturate them, because it's a product that they're already familiar with. It's so intuitive. And our patients have the exact same experience. Back when COVID was first ramping up, people were terrified. They were scared to reach out to help. And when they did reach out for help, it was generally because they had no other choice. So when they turned to us and they saw that we were attentive to their concerns and their fears, and that we had developed a technology that addressed those fears and increased their access to care, they embraced it instantly.
I can't tell you how awesome it feels to be at a farmer's market or in a grocery store and have somebody walk up and give you a big hug and say, ‘Thank you so much. Your team helped me. They helped my husband. They helped my father. They helped my mother.’ And it wouldn't have been possible without that [telehealth].
We do track satisfaction scores. On a scale of 1 to 5, where 5 indicates absolutely excellent service, what we're seeing is an average of 4.6 out of 5 on our satisfaction score. And that just tells me that the patients are relieved that we've added value to the services that we provide to them. That makes me feel great, and that makes my whole team feel great, because we feel like we're hitting the mark.
Dr. Jeremy DeWall:
One of the really interesting things that we found is, as James mentioned, we track a lot of data on this because it's a novel program for us. It was one of the first in the state to obviously start at a difficult time. We had a student out of the University of Phoenix Medical School who wanted to do a quality management project in emergency medicine or EMS. So she went through and pulled our initial data from 2020 to 2021, right in the beginning of the program. She reached out to as many of the patients or families as she possibly could through this study and reviewed that information through our quality management side.
She actually found that in general, patients within our communities—from urban to rural and frontier areas—don't like telehealth. They don't like the telehealth that comes with their insurance plan. They don't like the free one where you get the doc in a box that comes on and asks a couple of questions, and usually says, ‘You should see your doctor,’ or ‘You should go to the E.R.,’ or ‘You should go to an urgent care.’ We heard through this medical student that they really felt limited within the communities.
They liked this system because there was an EMS clinician present with them, whether they’re a community paramedic, an EMT, or a paramedic. They're touching them, listening to them, and communicating with a local physician that understands their community, their needs, and their difficulties. That made them comfortable, to where they actually really liked this system and said they liked it at least as much as going to the E.R. And typically, about 80% said they liked it better than going to the E.R., because it's quick.
So that's really what we saw. It was cool to see the data coming from the medical student looking at [the reasons] why there was that difference, because we didn't know the answer until she found it for us.
Q: What about the fire and EMS teams? They've been using Pulsara for EMS-to-ED communication. When you first started, how was integrating this new telehealth functionality into their existing workflows?
Dr. Jeremy DeWall:
It wasn't without hiccups, because everything new has hiccups. And quite frankly, it was us trying to figure out from a leadership perspective, from having leaders like James as well as other agency leaders really grasp it. That was, I think, our biggest challenge: this was completely new to EMS.
So we actually ended up developing a bunch of short videos on how to use it, giving examples. And quite frankly, what we started with is not what we do now. Some of it is; we've continued to improve it, both on the physician side, giving them feedback on the EMS clinician side and agency side, as well as on the technology side, working collaboratively as a team, saying, what's working, and what's not working? How do we improve this as a team? Which has been really wonderful.
So that was the challenge—initially getting the buy-in. We don't have full buy-in in all organizations that are doing it yet. James's team at Ute Pass Regional Health Service District were the first ones. There, we have great buy-in, and a very robust system to support it.
In some of the other agencies, it’s still that challenge of: I can have the patient sign a release of care, leave, and that's it. That takes less time, obviously.
Now, it takes less time to do telehealth than transporting a patient, as we can hit on later. But certainly, telehealth takes more time than ‘sign on the line and good luck with your life.’ If we did release of care, we'd quickly talk to them about risks, benefits, and alternatives. We'd sign a piece of paper, we'd leave, go do our PCR, and move on.
What has taken that time is to help our providers understand: there's more to this. We're really helping patients in their homes, and we’re really helping them navigate the health care system. And we're hopefully decreasing poor outcomes for those patients in the future, which I truly think we are, based on our data.

James McLaughlin:
Jeremy, I can't agree with you more. I think you absolutely hit one of the pinnacles of starting a new program: You just don't know what you don't know. You have a vision of how it should go and where things should go. But you have to be flexible and you have to have an amazing partnership.
And I will say we have an amazing partnership. You have to have that willingness to have those difficult conversations and say, ‘hey, look, this isn't quite working.’ And then you have to have the bravery to, you know, to pull something and change it. And the other important piece to that is you have to have a partner who's willing to pivot with you on a dime.
And that's what we've seen with Pulsara. When we'd have an issue and we'd say, ‘Hey, look, guys, I know we asked you to put time, effort, and energy into building this piece or putting that button in or putting that space to put information in, but now we need it to not only to collect the information, but we need it to push into our ePCR’ or ‘we need the ability to sign something’ or ‘we need the ability to add labs.’ And every time we came to them with an ask, they understood the importance of what was happening in our community and the importance of the need.
And they really were incredibly responsive. And our crews saw that. When you have a partner like that, it really allows you to not waste your time, effort, and energy on coming up with alternative ways to do something. You can just get it to do what you need it to do. And that allows you to put your your research and development energy into advancing the next piece or addressing the next quality assurance measure that needs to be addressed.
Dr. Jeremy DeWall:
We initially thought, oh boy, this should only be community paramedics doing this. James and I were both on that— 'This is going to take a lot of effort. It's going to be difficult.' But because it was utilized throughout our different agencies for different uses with notifying emergency departments, etc., now, we have BLS providers at volunteer transport agencies utilizing it. We have the ability for BLS volunteers at non-transport agencies as well as ALS folks to use [telehealth], on both sides of the volunteer and paid. That's been a huge enlightenment to us: telehealth doesn't have to just be [leveraged by] the transport agency. We can we can use it in multiple different ways.
James McLaughlin:
Well, and as the transport agency, it's a force multiplier for us, because these BLS transporting agencies, if they're not sure, their go-to is to reach out to us and request mutual aid from us. And we're not always the answer that the patient needs, honestly. And so it empowers those agencies to build a stronger partnership with the physician's group and to actually be the answer for the needs in their community.
And it allows us to keep our resources in our community and serve our community. So it's a win-win for everyone.
Q: The daily operations of a program like this are extremely important, as well as its sustainability. James, where did you get your doctors to be a part of this program, and why did you end up using EMS and emergency medicine docs instead of family practice or internal medicine?
James McLaughlin:
I’m so glad I have an opportunity to talk about this. Picking the right partners is imperative to any project or program that you bring to fruition. If you select the wrong people, it's going to be really hard to make it successful. We reached out to a lot of different partners, and we reached out to a lot of different physicians groups.
And at first, most of them had not the time, effort, or energy to even entertain the conversation so that we could share our vision and our idea. And of the few that did it, they didn't bring to the table the collaborative partnership that we desired. The doctors don't have all the answers, and the EMS providers don't have all the answers. It's when we come together, work in a meaningful way as a team, and communicate in an effective manner that we really accomplish great things.
And what was so awesome is the answer was right in front of our face. We had an amazing group of physicians that we worked with at the local emergency rooms. They knew us, we knew them. They knew each of our providers’ strengths and weaknesses. And we knew the nuances associated with those with those physicians. We already had a relationship. They saw our vision and understood what we were looking to accomplish. And they made our vision their vision from the beginning. It is really hard to find a partner that's willing to do that.
So when we had those initial conversations with George Hertner and a group from EMSPC, they heard the passion that we had to truly serve our community, which aligned with the passion they had to serve our community. So it was a perfect fit from the beginning, and they were willing to step up.
And I'll be honest with you, they are not covering the cost of the program at this point. You know, they're still not covering 100% of what they're putting into it. And yet the physicians continue to show up. They continue to fill those shifts. They continue to be available. And we're getting close. I know that we’ll be there soon. And they know that, too. But it hasn't come without some pain.
But we did look at other groups. We looked at using non-emergency physicians. And the reality is, is when you use board-certified emergency physicians, they understand what the E.R. can do, and what the E.R. isn't equipped for. They understand the rules and regulations around EMS. And so they're not going to put our agency or our providers in a position where they're going to be asked to do things or cosign things that just aren't safe for the patient.
And so that collaborative partnership and that understanding of one another's worlds has added so much value to the work that we do. And honestly, this collaborative relationship has made the relationship even stronger in the E.R.s, because now we come in and we see each other and we remember that amazing work we did for this patient who couldn't get the medications that they needed. Or, the behavioral health patient who was getting ready to run out of their medication, and they were terrified. They had nowhere to turn and they couldn't get a hold of their their physician, so they reached out to us as a last ditch effort. And we teamed up with our physicians and they were able to make that happen. I mean, it is not an exaggeration to say that this partnership changes lives. And I don't know that we would have seen that with another partnership.
Q: Has it helped with patient satisfaction to have the physicians actually be in-state?
James McLaughlin:
Absolutely. And that's a fantastic point. You know, there are other programs that use out-of-state physicians. And again, there's a difficulty to understand. You don't get that same value when you're working with a physician who doesn't know the nuances of your state and the resources that are available. Colorado has unique challenges, just like California has unique challenges, or like Florida has unique challenges.
And if that's all that's available, I think that's better than nothing. But if you can bring an in-state partner like we have here, I think there's real value to that.
Dr. Jeremy DeWall:
We've heard from agencies in parts of the United States that are really trying to develop a program, and they don't have any local partners that are willing or interested in doing it, or able to do it. Quite frankly, especially in some of these rural areas throughout America, you may not have an emergency medicine group that's close to you or even in-state that is looking at doing this.
In looking at a program and how to develop this into the future, I think the key is: In-state is helpful, but more importantly, you need a physician partner group that is willing to come and learn about your area. For example, right now, the same people that work with us, with our agencies, are on the other side of the state, actually working with another agency, developing their telehealth program.
And that agency has chosen to do that for that exact reason. They actually have a doctor out there who's learning about their challenges, their needs, their wants, how their community is set up, what their resources are. I think that's the key: finding a partner who is willing to meet you and learn about you.
And as James mentioned earlier, it's important to have those challenging conversations when they need to happen, and then bring that back to the rest of the team that's doing the telehealth so that it seems to the patient, regardless of where the docs are, that when you're on together, it's you together, working with that patient as a team to develop their care plan collaboratively. That's what I think is the magic in it.
Stay tuned for part 2, where McLaughlin and Dr. DeWall discuss the ins and outs of a good partnership and how telehealth can help increase the reach of small crews!
 Jeremy DeWall, MD, FAEMS, NRP, EMS Medical Director at UCHealth Pike's Peak Regional Hospital, CO
Jeremy DeWall, MD, FAEMS, NRP, EMS Medical Director at UCHealth Pike's Peak Regional Hospital, CO
Dr. Jeremy DeWall has been a Nationally Registered Paramedic since 1998 and currently practices as a board-certified emergency medicine and board-certified emergency medical services physician at UCHealth Pikes Peak Regional Hospital and Center for EMS Excellence in Woodland Park, Colorado. Over his many years of service and experience, Dr. DeWall has also worked as a flight physician, been a ski patroller with NSP for numerous years with extensive involvement in Outdoor Emergency Care and Mountain Travel and Rescue education through the National Ski Patrol, and volunteered as a firefighter and EMT.
As the dedicated Medical Director for the Pikes Peak, Southern, and Southeastern Colorado Regions, Dr. DeWall also supports 47 EMS services and nursing/camp programs ranging from EMS education services, tactical EMS services, mine rescue, urban and wilderness services, and nursing services. Dr. DeWall also provides regional medical direction for two Regional Trauma Advisory Councils and is a committee member for the State Emergency Medical and Trauma Advisory Council for the State of Colorado. He is also the Chief Executive Officer of Wilderness & Emergency Care Consulting, PLLC in Woodland Park, Colorado.
As an educator passionate about bringing evidence-based prehospital care and guidelines to providers, Dr. DeWall also trains medical students in emergency medicine and general medicine at the University of Colorado Medical School. In 2020, he was recognized for his continued commitment to prehospital emergency care by acceptance as a Fellow of the Academy of Emergency Medical Services (FAEMS).
 James McLaughlin, Director of Community Paramedicine at Ute Pass Regional Health Service District
James McLaughlin, Director of Community Paramedicine at Ute Pass Regional Health Service District
James (TINY) McLaughlin is the Director of Community Paramedicine at Ute Pass Regional Health Service District in the Colorado Springs, Colorado Area. Aside from his responsibilities to the district, James has served three terms as President of the Teller County Emergency Medical Service Council. He also serves as chairman of the Pikes Peak Community College Emergency Medical Service Advisory Committee and is a founding member of the Teller County Mental Health Alliance.
As an adjunct faculty member for Pikes Peak Community College, James is also the lead instructor for the International Community Paramedic Program. He also teaches for the University of Colorado Health Center for EMS Excellence and is a former instructor for the prestigious Penrose St. Francis Institute.
 Cara McCoy, CS Specialist with Pulsara and former Fire Engineer and EMT
Cara McCoy, CS Specialist with Pulsara and former Fire Engineer and EMT
With experience as both a firefighter and EMT, Cara McCoy brings over a decade of fire rescue, clinical, and leadership experience to her role as a Customer Success Specialist for Pulsara.
After first developing a passion for emergency response in high school as a volunteer at her local fire department, Cara began her fire rescue career in 2010 with New Hanover County Fire Rescue in North Carolina. Her skills and experience quickly grew as she gained certifications as a Firefighter, EMT, Driver Operator, and Technical Rescuer. In 2012 she moved back to her hometown of Raleigh and began working as a Firefighter/EMT with nearby Cary Fire Department. Honing her skills and experience over the next few years, Cara became a Fire Engineer in 2020. From 2014 to 2021, Cara also served her local community as an EMT on Rex Hospital’s Emergency Response Team.
Today, Cara brings her deep passion for patient care to Pulsara as a Customer Success Specialist for the Western US. Cara trains and supports Pulsara customers along the whole patient care continuum, including fire, EMS, and hospital systems to better serve their communities through united care teams.
![]()
With a scalable system of care, Austin-Travis County EMS kept 434 low-acuity patients out of the hospital over just three weeks—and rerouted them to faster, more appropriate care. Here's how they did it.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...