Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

EDITOR'S NOTE: This article originally appeared on FireRescue1.com. Special thanks to our guest author, Courtney Levin, for FireRescue1 BrandFocus Staff.
Departments can play a large role in supporting the health and safety of underserved residents
The inherent nature of the fire service means that responses to community needs are usually reactive. Whether a 911 call is for a fire, a serious vehicle collision, or a medical emergency at someone’s home, firefighters can’t predict ahead of time where these instances will occur.
That’s not to say the fire service hasn’t made great strides to be proactive about their day-to-day operations when and where they can. For example, departments routinely engage in fire inspections to bolster the safety of local buildings. After all, reducing the likelihood of a fire starting is certainly a more preventative route to take than fighting a fire once it’s begun.
Proactivity isn’t limited to structure fires, though. Fire departments can also apply this line of thinking to the individual residents in their community by developing a community paramedicine program.
[While we are using the term “community paramedicine” for simplicity, there are other similar terms, including “mobile integrated health” and “community integrated health.”]
Many EMS agencies across the country already engage in community paramedicine programs, and the fire service can and should play an important role in those programs. Whether your area already has this type of care in place or not, there’s always an opportunity to provide greater support for the underserved residents in your community.
Before putting pencil to paper and determining how to structure your community paramedicine program, it’s essential to have a conversation with every member of your department – from top leadership all the way down to newly hired staff and volunteers.
“If you don’t have an executive vision and leadership for how you want to grow your department from a chief level or a senior leadership level, it’s not going to trickle down all the way through,” said Kris Kaull, chief growth officer at Pulsara. “And in the same way, the value of why we’re committed to a community paramedicine program needs to be shared across all ranks.”
These discussions can begin at a basic level, like asking questions such as, “Why do we exist as a fire service?” and “What is our value to the community?” By reaffirming these foundational motivations, departments can start to bring everyone into alignment around the implementation of a community paramedicine program.
Kaull says a culture of innovation is key to launching a successful program, as this new way of looking at serving the community may substantially differ from the way a department has always done things.
It’s also critical to find champions of community paramedicine in areas beyond your fire department. Partnering with experts within the local emergency department or those from social services can add value to the program.
Simply saying, “We’re going to start a community paramedicine program” is too broad a goal for any fire department. Instead, complete a needs assessment for your community and identify specific and actionable goals. As a first step in the planning process, it may be beneficial to examine existing programs and gather additional stakeholders, such as community preparedness, social workers, and mental wellness experts.
Before starting, ask around. There are many fire departments across the nation who’ve been working through these challenges for years. “There are people out there who are already doing a great job of this. I encourage departments to reach out, network, and learn from others,” said Kaull. “Departments should also consider creating an advisory group and including stakeholders from the community who need to be part of the program.”
Gathering lessons learned from outside sources, while also considering their own observations when running calls, can help firefighters determine what their community needs the most. Establishing a baseline of what’s going on – for instance, how many calls are for fall assists, how many are for mental health, and how many are related to houselessness – provides insight into where a community paramedicine program should focus its efforts, explains Kaull.
“Then start asking, ‘What’s the burden on the emergency department? If we had other alternative locations to treat patients, what are the opportunities to help reduce emergency department wait times?’” Kaull said. “The needs in your area are unique – they’re different in San Francisco than they are in Dallas, Texas. They’re different in a rural community than they may be in a suburban setting.”
Though your team might come up with many ideas to tackle, departments tend to have the most success when they start small. Consider brainstorming ten aspects to include in your community paramedicine program and see what sticks. If you find that three are successful, dig into those three. Then, slowly add other services as your program grows.
“What’s one thing your department could do that would make a difference in your community? Start with that. Look at the data. Build a program. Measure your success.” said Kaull. “Then continuously expand the program as health care needs change.”
While a fire department might find that their community’s needs differ significantly compared to their neighboring department, some prevailing themes tend to pop up within community paramedicine programs.
For example, you may find your department prioritizing fall prevention. If local nursing homes are calling 911 regularly due to residents slipping or tripping, your department might want to take preventative action to mitigate risk. Removing rugs and other hazards can help increase safety for residents and reduce the number of calls related to these incidents.
Other situations might be more patient-specific, shares Kaull.
“When looking at their run data, one department saw that they continued transporting the same patient to the emergency room for diabetic-related issues,” he described. “In a proactive manner, they reached out to the patient and discovered that the patient’s insurance no longer covered their insulin medication and they couldn’t afford it.”
A member of that fire crew then spoke with the patient’s physician, who was unaware of the issue. The physician changed the patient’s prescription to a medication that would be covered by insurance, and the patient no longer needed to regularly call 911 for medical care.
Scenarios like these are what’s at the heart of community paramedicine. Instead of transporting the same patient to the hospital repeatedly and not addressing the underlying problem, fire crews can take proactive measures to ensure the needs of their community are being met.
As with any call, communication is critical to achieving successful patient outcomes. Whether mitigating the risk of falling or working with a patient to change their medication, fire crews can use the Pulsara platform to streamline their efforts.
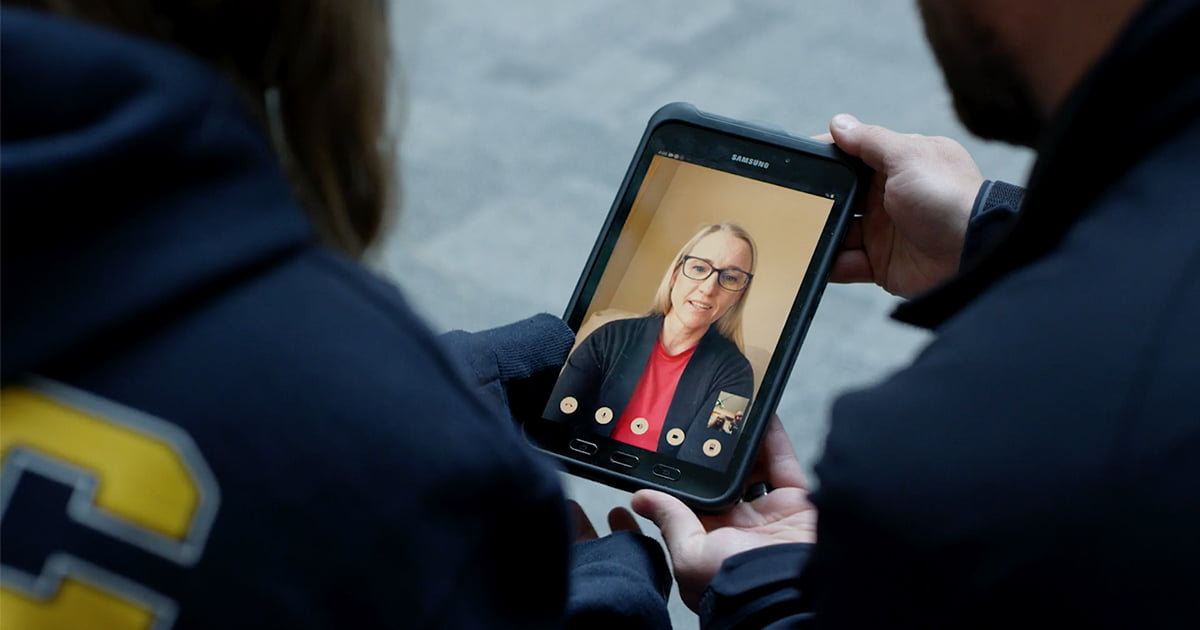
“In the simplest terms, I always think of Pulsara as a HIPAA-compliant, safe way to communicate,” said Kaull. “I can start a case for a patient, and then as the case dynamically evolves, I can bring in other resources as needed. It’s as simple as using WhatsApp, Amazon or FaceTime.”
Many times, a patient’s condition may not be critical or time-sensitive, but still complex in nature. Through Pulsara, those on scene can have a real-time dialogue with others, including their medical direction, someone from social services, or the patient’s primary care physician. By working together, the fire department is truly meeting the needs of the patient and not merely responding to an incident.
“A patient may not necessarily need to go to the hospital but may benefit from being seen at an alternative destination,” said Kaull. “A conversation and real-time consult through Pulsara with medical direction may prove helpful in this example. We’ve seen great things when departments use Pulsara to loop in experts for mental health and wellness patients.”
No matter how simple or complex your community paramedicine program becomes, tools like Pulsara can help ensure better communication and ultimately, better outcomes for your patients.
“In the fire service, we use archaic technology to manage complex problems, like pagers, handheld radios, and answering services,” explained Kaull. “And yet, in real life, we use our phones to communicate dynamically. With Pulsara, you can save all of the unnecessary headaches and more appropriately treat the patient’s needs.”
![]()
Once you've laid the groundwork for your community paramedicine program, there are more practical steps you can take to make your program a success. Check out our follow-up post, Community Paramedicine And The Fire Service: Making Your Plan Work.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...