Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
EDITOR'S NOTE: Special thanks to Kinsie Clarkson (Pulsara's Product Marketing Specialist, 2020-2025) for writing today's blog post. You can connect with her on LinkedIn.
__
Chaos is woven into the DNA of emergent care. Emergency care professionals face the unknown around every corner—from supporting a low acuity patient to managing a mass casualty event. You never know what you’re going to get.
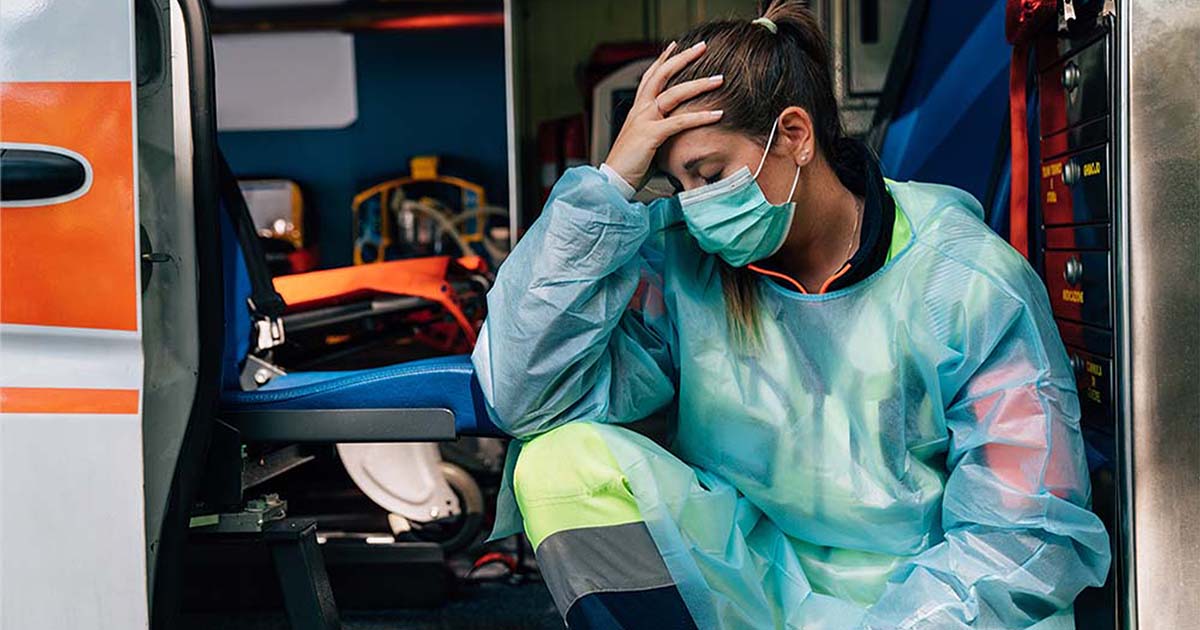
Sometimes, you have a day that’s more chaotic than others. Other times, the chaos lasts much longer than a day—it can become a lasting situation that extends into months and even years. Few seasons have been quite as chaotic as the COVID-19 pandemic. COVID has tested and tried our healthcare systems to the breaking point, introducing factors like virus spikes, hospitalization surges, burnout, and staffing shortages.
To keep growing, keep improving, and keep adapting to the situation, some things will need to change. The problem is, it seems impossible to do anything about the situation while you’re treading water. It can feel like trying to bail out a rowboat as you continue to paddle—trying to do everything all at the same time. But if you can introduce a change that will help either paddle the boat or bail with less effort, the time and energy it takes to implement that change will ultimately help make the job easier for the long term.
The pandemic has caused many in healthcare to realize that our current processes for communication in healthcare aren’t sustainable. When we try to communicate outside our standard day-to-day patterns using the same technologies we always have, they don’t give us the transparency or ease of communication that we need to respond quickly. In order to effectively handle large-scale emergency situations, we need to create new connections and communicate with people we don’t usually talk to—preferably in a familiar way that doesn’t require us to learn a new system.

As we face surges and staffing shortages, it’s never been more important for team members to be able to connect with one another and exchange detailed information quickly, efficiently, and correctly. We need to be able to support patients from a distance, and we need to be able to see critical needs across our region and easily transfer patients in need to the places that have the resources to care for them. We need a reliable system that can help us stay in touch with each other: something that can match our needs at the moment, whatever the next moment brings.
The good news is that this solution exists, and we’re here to help. Pulsara is all about successful change management, and we’re here to walk with you as you move towards improved patient care. Whether you’re thinking about using Pulsara or making any other change to your current processes, here are some of the significant concerns that arise when managing change amid chaos, as well as practical tips you can put into practice when talking with your team about change management.
The middle of a chaotic situation certainly doesn’t seem like a good time to try a new way of doing things. There are all sorts of variables: overwhelmed resources, not enough beds, not enough staff, surges of new patients, new variants—
Forget optimization. You’re just trying to keep the wheels on.
In certain situations, though, making changes to the current system can help relieve some of the pressure on your overworked, overwhelmed, overburdened system.

When it comes to healthcare communication, the change can’t wait for the crisis to end. The learning curve might seem steep, but Pulsara was designed to be intuitive and easy to use. Most people already use smartphones to communicate for almost everything in life—from texting with family and friends to ordering a pizza. Pulsara has been designed with those same familiar user experiences in mind, making it intuitive to learn and easy to use.
Change in a crisis is hard. Taking the time to alter course can seem like the straw that will break the camel’s back. But if you take the time to adjust, you might find that it provides not only some much-needed relief, but also other benefits like streamlined workflows, higher team collaboration and morale, and ultimately, improved patient outcomes.
Change is challenging under the best of circumstances. During chaotic periods, you’re going to encounter even more resistance. Chances are, your team members are in survival mode. They’re tired. They’re burnt out. They’ve had it, and they’re not sure how much longer they can hold on. They don’t have much of an appetite for change. Even the suggestion of trying something new seems like yet one more mountain they don’t have the energy to climb.
They can’t yet see the light at the end of the tunnel—but you can see a glimmer. You may not be able to see the end of the situation or the solution that will solve everything, but you do have an idea for how to institute a change that might make things a little easier. You can see a spark of hope.

In order to create lasting change, you’ll need to get everyone on board with the vision. To create buy-in, it is essential to help your team see that spark of hope, too. Hosting stakeholder meetings that include everyone affected by the change is a great way to communicate the why and help others see the vision. Explain the reasons for the decision and how it will help them deliver better patient care. They need to understand the “why” behind the change. What is this going to accomplish? How is it going to make life easier for them? And ultimately, why are you doing it?
Once everyone understands the vision, how this will benefit their patients, and ultimately make their lives easier, they’ll be more willing to give it a try.
While it will be difficult, try to be patient with those who continually hold out and refuse to cooperate. Chances are, it’s more out of fear and fatigue than from any real objections to your goals. After all, we all want better care for patients, right? Once everyone understands how the plan will happen and how they fit into the big picture, they’ll be more motivated to participate.
In the middle of chaos, it’s also common for team members to feel overworked, overwhelmed, and underappreciated. They may be more inclined to feel that new changes will complicate their lives, especially if they don’t have the opportunity to participate in the decision-making process. Try to listen to concerns, understand where they’re coming from, and allow everyone the chance to have their voices heard. Once team members feel that their concerns matter and have been taken into consideration, they’ll be more willing to try out the solution you’re proposing.
If your team is thinking about switching to Pulsara, the prospect may seem intimidating or daunting—especially if you’re in the middle of a surge event or extra workplace stress. Knowing the ins and outs of your system as you do, it may even feel impossible. It may feel like too much time, too much effort, and too many people involved to try and implement what feels like such a large-scale change.
But here’s the good news. You’re not facing this daunting task alone. (And it may be easier than you think.)
If you’re considering coming on board with Pulsara, rest assured that we will walk with you through this every step of the way. We see our relationship with every customer as a partnership, and we’re committed to providing you with the resources and reinforcement you need to help your teams succeed. If you’re worried about collaborating with neighboring organizations, don’t stress—we’ll initiate conversations with them and take care of their questions, implementation and onboarding needs, and training.

Pulsara is a light technology lift that’s easy to implement because you’re already familiar with the user experience. Our software is intuitive because it follows the same user experience you have every day as you use your smartphone to communicate with your friends and loved ones. Our customers regularly rave about how easy Pulsara is to implement and learn to use.
You’re on the front lines fighting this pandemic and trying to provide care for your patients. Our goal is to make that goal easier for you—and that includes the process of making this change happen.
The State of Texas and the State of Arkansas are using Pulsara to solve load balancing issues due to COVID-19. Check out what Pulsara MED OPS can do for you.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...