Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, Marianne Meyers, BS, for EMS1 BrandFocus.
__
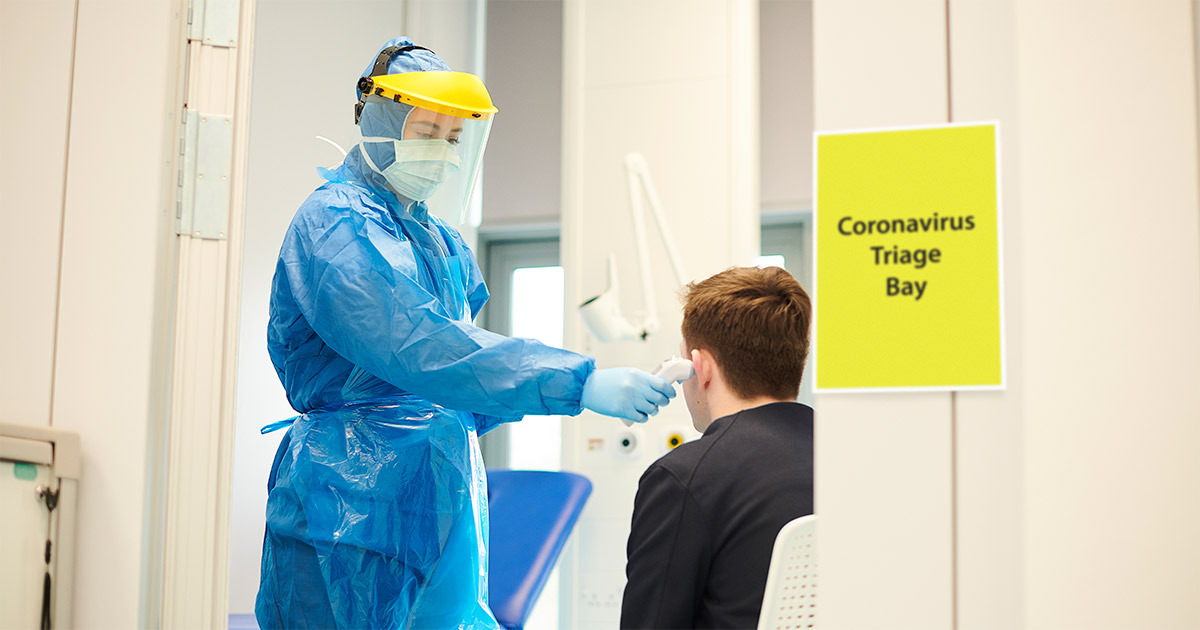
As 2021 begins, COVID-19 vaccines have recently been approved, and it appears that the beginning of the pandemic’s end is in sight. That said, we are still experiencing large spikes throughout the country, and hospitals and EMS systems are under immense strain.
We aren’t quite on the other side, but we can now see the light at the end of the tunnel.
Here are 10 things we’ve learned from the pandemic that can help improve other areas of EMS response:
 Telemedicine was underutilized prior to COVID-19, and it is almost certain to become more common in the future. During the pandemic, physicians needed a way to continue to see patients while minimizing the risks of exposure to COVID-19. Telemedicine quickly became the clear solution. Virtual appointments allowed patients to get advice from physicians without exposing everyone in the waiting room.
Telemedicine was underutilized prior to COVID-19, and it is almost certain to become more common in the future. During the pandemic, physicians needed a way to continue to see patients while minimizing the risks of exposure to COVID-19. Telemedicine quickly became the clear solution. Virtual appointments allowed patients to get advice from physicians without exposing everyone in the waiting room.
Telemedicine has historically been underutilized in EMS as well, and it’s something we should take advantage of in the future. Companies like Pulsara have developed applications that allow EMS providers and patients to communicate directly with hospitals and physicians, helping them develop treatment plans and provide the best care for the patient.
As first responders, we are at higher risk of infection because of the nature of our work. But with the proper protection, we can help prevent transmission. One study from Seattle showed that less than 0.5% of EMS providers tested positive for COVID-19 two weeks after exposure to a confirmed positive patient. Other studies have shown that N95 respirators adequately protect the wearer against viral particles.
Proper PPE will help protect you from the virus. At minimum, an N95 mask and eye protection should be worn with every suspected COVID patient.

Wearing masks and staying socially distanced from one another helps prevent the spread of the virus. Several studies have shown that there is a significant risk reduction of COVID-19 infection with even just a cloth mask or neck gaiter. Along with physical distancing, masks help cut down on virus transmission.
Many people still deny that COVID-19 is a problem, or even real to begin with. Many refuse to change their daily routine, wear masks or keep their distance. Many more are skeptical of the new vaccines.
As healthcare providers, we understand the science behind the recommendations and have seen firsthand how devastating this virus can be. Our job should not only be to help those in need, but to educate those about what we’re facing and what tools we have to combat it.
Answering questions and explaining practices to non-medical personnel with patience and kindness can help turn skeptics into believers armed with information they can share with their friends and family.
.png?width=276&name=COVID-19-Goal-3-Limit-Exposure(1).png) Some COVID-19 presentations may be obvious, but others may not. The classic symptoms of fever, cough, and shortness of breath may not be present in every patient. Other symptoms may be predominant. Headache, diarrhea, vomiting, body aches, fatigue, loss of taste or smell, and congestion are all possible symptoms of the virus.
Some COVID-19 presentations may be obvious, but others may not. The classic symptoms of fever, cough, and shortness of breath may not be present in every patient. Other symptoms may be predominant. Headache, diarrhea, vomiting, body aches, fatigue, loss of taste or smell, and congestion are all possible symptoms of the virus.
Whether or not it seems likely that you or someone you know has contracted COVID-19, don’t rule it out based only on symptoms. It’s still important to ask about possible sick contacts, travel, and other potential risk factors for exposure.
First responders have always had stressful jobs, but now their jobs have become even more difficult. This is a stressful and scary time, especially for those in healthcare who are putting their lives – and their families’ health – at risk.
It’s important to be aware of the toll stress can take on your well-being. Take the time to take care of yourself and your mental health. Talk to others about how you’re feeling. Go for a walk, read a book, debrief with peers about hard cases you’ve faced together, and try to do something every day that makes you happy.
 COVID-19 showed us many areas we were not prepared to handle a pandemic – lack of sufficient equipment is just one example. We all experienced feelings of fear and frustration when we realized that single-use masks were going to have to be reused – and worse, that there may not even be enough protective equipment to go around.
COVID-19 showed us many areas we were not prepared to handle a pandemic – lack of sufficient equipment is just one example. We all experienced feelings of fear and frustration when we realized that single-use masks were going to have to be reused – and worse, that there may not even be enough protective equipment to go around.
This shouldn’t have happened. Our next step should be to learn from the experience. Hospitals, states, and healthcare organizations – including EMS agencies – need to prioritize preparing and stockpiling protective equipment for the next big illness. The next pandemic isn’t an if, but a when, and we can use the COVID-19 pandemic as a learning experience to improve our response to the next one.
Companies have managed to develop a COVID-19 vaccine in less than a year, shattering all previous vaccine timelines.
Traditional methods for developing vaccines use live or dead virus DNA to help the body recognize and attack the virus. These vaccines take longer to develop, and some carry the risk of infecting the patient with the bug they were attempting to protect them from.
 Taking a brief trip back to college biology (sorry): DNA is translated into mRNA, then transcribed into proteins. In the case of the vaccine, these proteins are antigens that the body’s immune cells react to.
Taking a brief trip back to college biology (sorry): DNA is translated into mRNA, then transcribed into proteins. In the case of the vaccine, these proteins are antigens that the body’s immune cells react to.
Compared to traditional vaccines, mRNA activates more of the body’s immune response and can be manufactured faster. The new COVID-19 vaccines mark the first time mRNA vaccines have been used in a large-scale setting, and based on their trials, they are about to be a huge success. This means we will probably see more mRNA-based vaccines and therapies in the future.
Everyone is tired of dealing with COVID-19 – but that doesn’t mean we can let our guard down. It is incredibly tempting to see friends and family outside your household, skip the mask, and return to more normal living.
Unfortunately, we can’t go back to the way things were just yet. Take the time to gear up correctly – every time – and think about every action you perform and how you may be putting yourself and others at risk.
Throughout the year, there have been countless stories of courage, kindness, and resilience from people around the world. Everyone has been stepping up to help their neighbors and do what they can to support healthcare workers.

I may be biased, but I believe healthcare providers (especially EMS) have been incredibly brave, and they have spent this year working harder than ever. Despite overwhelming patient volumes, lack of resources, risks to self, and the fact that little was known about the virus, they continued to show up to do everything they could for their patients.
To all my fellow healthcare workers: Thank you. You’ve shown a great deal of courage and selflessness this year, and we are all grateful for you.
About the Author
Marianne Meyers, BS, is a third-year medical student at the University of Washington School of Medicine interested in pursuing emergency medicine. Previously, she was a member of the Santa Clara University collegiate EMS squad where she received her B.S. in Public Health Science. Additionally, she has worked with the King County Public Health Department in Seattle, Washington, studying EMT naloxone administration.
For leading EMS organizations, telehealth has been a major resource for helping manage the COVID-19 surge. Check out How Video Streaming Benefits Everyone Involved in an EMS Call to learn more.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...