3 min read
In the News: Pulsara's Impact in Colorado, Texas, and Scotland
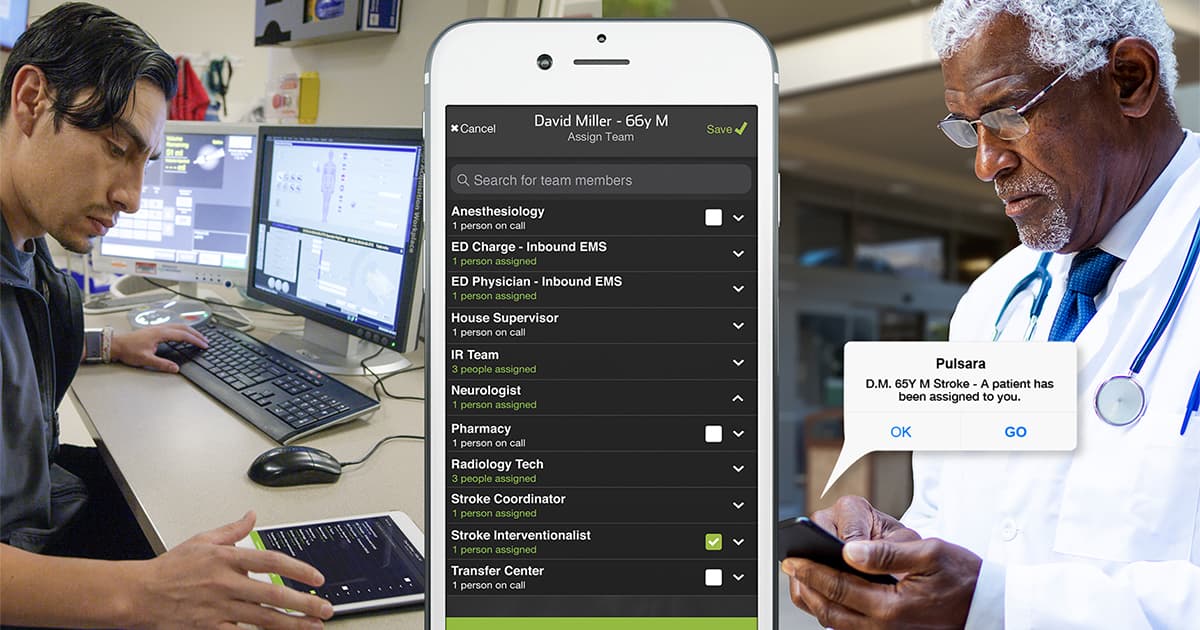
At Pulsara, our customers are why we do what we do. It's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. Several of our customers have...