Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
![The State of the Profession [2020 EMS Trend Report Part 1]](https://www.pulsara.com/hubfs/ems-background-1200x630.jpg)
EDITOR'S NOTE: Last month, EMS1, Fitch & Associates, and the National EMS Management Association released their third annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS.
About the authors: Jay Fitch, PhD, is a founding partner of Fitch & Associates and is internationally recognized for leadership as a consultant, educator and innovator in EMS and public safety.
Anthony Minge, EdD, is a senior partner at Fitch & Associates. Prior to joining the firm, he was the business manager for Northwest MedStar in Spokane, Washington.
—EMS leaders anticipated a linear progression in 2020 – managing a slight increase in call volume and reimbursement, while trying to become more efficient and otherwise hold down costs. COVID-19 certainly changed the definition of normal, and perhaps how EMS will evolve in the future.
The EMS Trend Report asks a number of questions each year to ascertain industry perception of a wide variety of key issues and related trends, from measures used to track cardiac arrests, to clinical interventions, ePCR satisfaction, use of lights and sirens for 911 responses, budget changes, and the degree to which agencies are prepared for disruptive events.
When asked, “Which, if any, measures does your organization calculate and track for cardiac arrest?,” the majority of respondents across all service types (61%) report that they measure return of spontaneous circulation (ROSC). A smaller percentage (37%) of respondents indicate they measure survival to discharge. Only 14% report that they use a cerebral performance category (CPC) score, while nearly a third of respondents across all service types (31%) indicate they don’t know what their service uses.
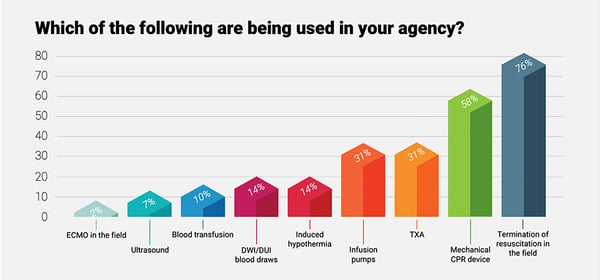
Respondents were also asked about clinical modalities, equipment and protocols adopted by their agencies. The percentage of treatment modality usage overall has remained relatively constant in recent years, but as we looked more closely at the data, several trends emerge.
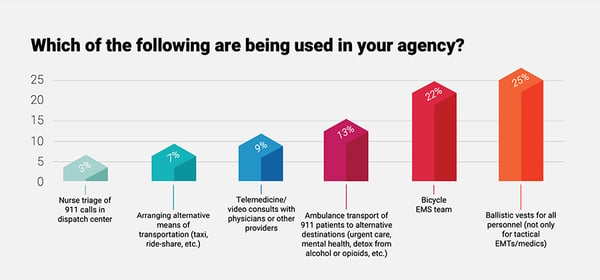
One of the most notable findings is the high frequency of adoption/use by hospital-based service models. Additional cross-tabulations revealed a distinct correlation between medical director engagement and the number of adopted clinical modalities. While the data infrastructure of participating systems does not allow a direct correlation to actual patient outcomes, the key take-away for EMS leaders is that when the medical director is more actively involved with the service, additional treatment modalities are often adopted and available for patients.
 EPCRS SATISFACTION
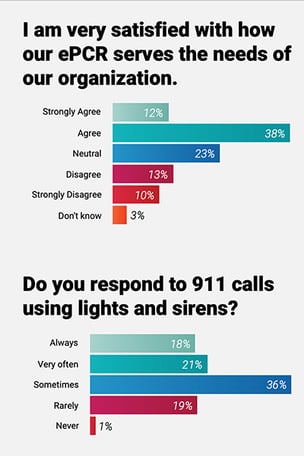
EPCRS SATISFACTIONWhen asked how their electronic patient care reporting system meets the needs of their organizations, managers were almost twice as likely as field providers to strongly agree that they were satisfied, and nearly four times more likely than educators and medical directors. Managers rated 18.9% compared to 10% by field personnel, 5% by educators and 5.6% by medical directors responding to the survey.
Fire department-based respondents continue to report the highest rates of using lights and sirens for every call (25%, compared to a 15% average in other agency types). Based on published research questioning the efficacy of responding lights and responses to all 911 calls, and the inherent dangers, this points to a policy and training opportunity to improve patient, provider and community safety.
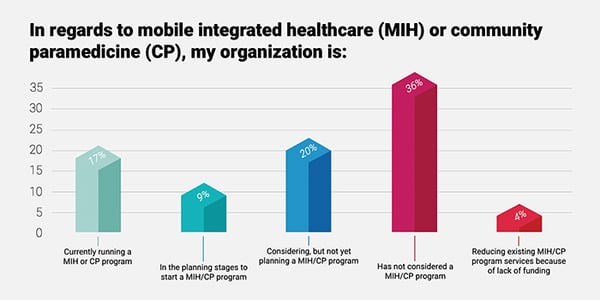
Despite the excitement about the Center for Medicare and Medicaid Services announcement of the Emergency Triage, Treat, and Transport (ET-3) pilot project last year, the percent of respondents that are operating or planning a mobile integrated healthcare (MIH) or community paramedicine (CP) program declined over the past three years from 33% in 2018 to 25% in 2020. When broken down by type of service, hospitals and third services report the highest percentage of MIH or CP programs this year.
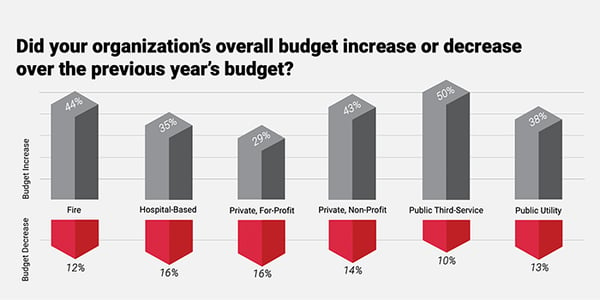
When measured across all agency types, 60% of respondents indicated EMS budgets increased or remained the same in the past year. Fourteen percent of respondents indicated budgets decreased, while 25% of respondents indicated they did not know.
The survey closed before the full impact of COVID-19 was fully realized. Ambulance volumes nationwide were reported to have initially declined dramatically but have recently increased as more healthcare facilities are re-opening and providing surgery and other inpatient services. Return to a normal state (whatever that is) will not be a reality for some time.
Based on local government’s declining sales and property tax revenues, and unemployment figures that may indicate an increasing number of non-insured patients, changes in revenue and expense budgets will be key trends to observe in the coming year.
While medical directors believe that they are very engaged with field personnel (7 in 10 strongly agree) only 2 in 10 medics and EMTs agree. In the open-ended field, respondents highly valued face-to-face interaction and “street time,” in engaged directors.
Others noted they only encountered their medical director at annual refresher training, or in disciplinary matters. Worse yet, numerous respondents indicated they don’t know who their medical director is, or what they do. Many identified a decline in interaction over time, where the medical director started out strong, and then stopped putting in the effort to meet with providers.
While field personnel may not be aware of all the medical director’s activities, it is clear that
if perceptions are reality, then there is some heavy lifting to be done to change caregiver perceptions about medical director engagement and to preserve that important relationship.

At the outset of our 2020 analysis, we noted two foreboding factors related to the future of the EMS profession. Over the last 3 years, there has been a significant downward trend of those that would recommend EMS as a career for their children or other young people and those optimistic about the future of EMS. In 2018, nearly 9 of 10 respondents (88%) said they would recommend EMS. In 2020, that number had dropped by almost a third to slightly more than 6 in 10 (61%).
Career satisfaction is a major driver for recruitment and retention and the willingness to recommend EMS as a career is a strong indicator of career satisfaction. Similarly, another concerning trend is the number of respondents reporting that they are optimistic about the future of the profession. Positive responses fell from nearly two-thirds (65%) in 2018 to approximately half the respondents (50%) this year. These overarching satisfaction and optimism trends compel leaders to contemplate what needs to be done to address the changing perceptions.
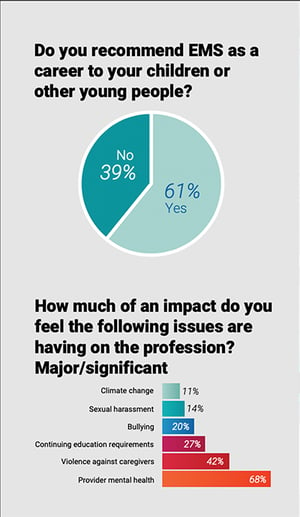
The way we care for caregivers in EMS continues to be a concern. In the 5 years of the EMS Trend Report, we’ve asked a series of pointed questions related to sexual harassment, bullying, clinician safety and provider mental health. The percentage of respondents who have indicated that sexual harassment is a major or significant issue impacting EMS has remained constant between 14% and 17%. The perception of bullying as a major or significant issue increased from 15% to 20% during the same period. In addition to concerns about caregiver safety, patient safety was consistently rated as a major or significant factor by more than 75% of the respondents.
Identifying provider mental health as a major or significant issue impacting EMS has increased for all respondents from 61% to 68% overall during the past 3 years. While awareness about mental wellness and suicide prevention has expanded in recent years, the fact that more than two-thirds of Trend Report respondents indicate it is a significant issue indicates that much remains to be done.
This year, the impact of mental health on the profession was rated highest by dispatchers (73%) and educators (74%). For 911 center professionals, there are a number of nasty realities that may contribute to this high rating. According to Jim Marshall, in his recent book “The Resilient 911 Professional,” contributing factors include:
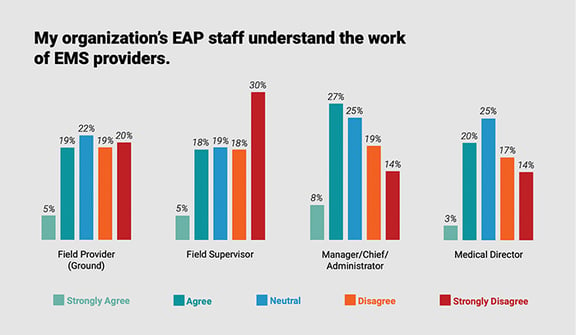
Responding managers and field personnel expressed diverse views about the effectiveness of employee assistance programs (EAPs). In this year’s survey, 35% of managers or chiefs agree or strongly agree with the statement that, “my organization’s employee assistance program (EAP) staff understand the work of EMS providers.” In contrast, 48% of field supervisors disagree or strongly disagree with the same statement. A number of respondents commented on the reluctance to use EAPs, the perception of a lack of confidentiality, the lack of EAP staff knowledge about EMS, and the short- term nature of EAP program services.
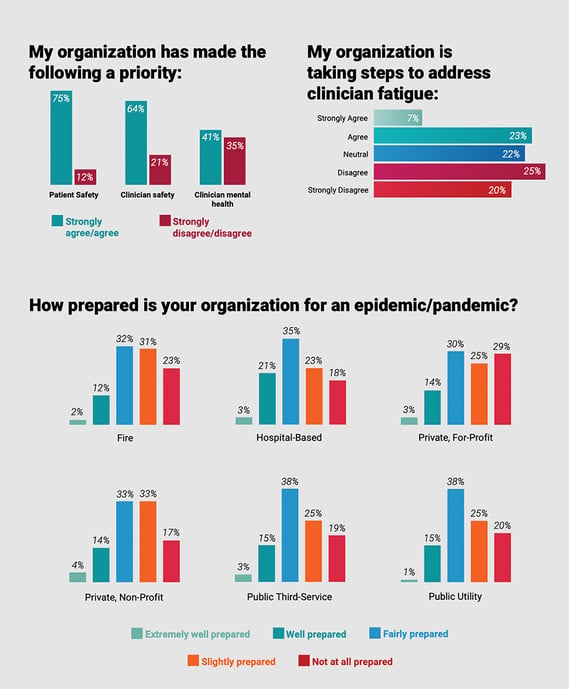
Fatigue management is another area in which there is a striking difference in responses between management and field personnel. Over half (52%) of managers agree or strongly agree with the statement “my organization is taking steps to address clinician fatigue,” while 56% of field providers disagree or strongly disagree with the statement. Looking across agencies, the percent of all respondents that agree or strongly agree their organization is addressing clinician fatigue has declined from 40% in 2018 to 31% in 2020. EMS organizations may find it helpful to begin to measure this dynamic internally and begin a dialogue discerning the underlying difference in perceptions to better address provider’s concerns.
Most responses to this year’s EMS Trend Report responses were received before the impact of COVID-19 was fully felt. It will be interesting to see how the pandemic influences perceptions within the profession in future years.

One of the most telling questions in the 2020 EMS Trend Report asked about pandemic preparedness. Only 15% of respondents across all service models believed their agencies are well prepared for an epidemic or pandemic, and the shortages of personal protective equipment, and scramble to outline quarantine and staffing measures supports the contention. We were clearly not ready.
During the first few months of the pandemic response, for the first time in the history of our profession, a paramedic, Alanna Badgley, was featured on the cover of “Time.” But beyond that, recognition for the incredibly difficult tasks of managing the EMS response was limited. EMS agencies and caregivers were largely forgotten among the healthcare heroes celebrated on the nightly news at the height of COVID-19.
Field providers were afraid to go home, for fear of exposing vulnerable family members. Many experienced the unanticipated stress of interacting with patients’ loved ones, who knew they would not be allowed to visit at the hospital and were saying tearful goodbyes in the back of the ambulance.
Despite the PPE shortage, the quarantines, the staffing concerns and the emotional toll, EMS continued to perform.
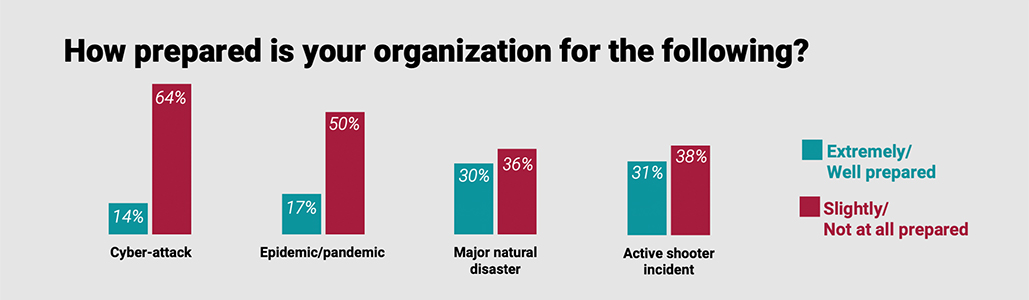
Respondents’ perceptions of agency readiness to overcome other risk factors should also give EMS leaders pause. Over the past 3 years, the responses have not shifted dramatically, continuing to indicate that managing the unexpected may be problematic.
Noteworthy among the survey responses were preparedness for active shooters and cyber attacks.
The percentage of respondents answering the question: “How prepared is your organization
for an Active Shooter incident” has remained constant over the past three years. Each year, 6% respond that they are “extremely well prepared” and between 23% and 24% indicate that their agencies are “well prepared.”
Few respondents believe that their agency is prepared for a cyber attack. On average, 11%
of all service models rate their agency as “well prepared.” Hospital-based service models rated themselves slightly higher (17%), perhaps due to their access to healthcare network/hospital IT resources and the emphasis on HIPAA and the automation of patient records.
As the EMS Trend Report enters its sixth year in 2021, we look forward to being able to report movement on key trends and perceptions. While we hope that COVID-19 is well behind us at that point, we will continue to monitor its current and longer-term impact on EMS.
Download the full 2020 EMS Trend Report here.
For the latest stats on the state of the EMS profession in 2020, check out part 2, part 3, and part 4, and part 5 of our 2020 EMS Trend Report coverage.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...