Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Editor's Update: The ET3 program is mentioned in the below report. Please note that, as reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
Editor's Note: On August 11th, EMS1, Fitch & Associates, and the National EMS Management Association released their fourth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is written by Anthony Minge, EdD, senior partner at Fitch & Associates.
How EMS is poised to tackle the challenges ahead after the greatest public health threat in generations
There’s no doubt that COVID-19 has had an impact on the profession. From call volume, to protective equipment, to technology adaptation, many things changed in between our 2020 and 2021 surveys. But what impact did COVID-19 have on the EMS community’s perception of itself? The answer, of course, is not simple. But the quick summary? Not as much impact as we might have thought.
On reflection, though, perhaps that isn’t very surprising. The challenges wrought on EMS by COVID-19 were unique in some ways – the need for more PPE, an incredible campaign to vaccinate the workforce – but mostly, the same challenges EMS has faced for years, if not decades: an overworked, fatigued workforce; reimbursement schemes that can’t sustain a people-centered system; inadequate coordination between EMS, public health, and healthcare. These challenges have always been there; just look at the five previous years of the EMS Trend Report. COVID-19, however, has accelerated these challenges, pushing some clinicians and organizations to the brink. But it has also raised the profile of EMS, perhaps creating opportunities to engage with healthcare, community and political leadership to finally get the change we’ve been asking for, for far too long.
Perhaps no question is more telling about how EMS professionals feel about the profession than whether they would recommend EMS as a career to the next generation. Despite reports that COVID-19 and the associated dangers might drive people away from the profession, survey respondents were just as likely to say they would encourage people to enter the field as they were in 2020. As in 2020, 61% of respondents in 2021 noted they would recommend EMS, while just under 40% wouldn’t. Also, that question reveals the same disconnect between leadership and field providers, with medical directors most likely to recommend (83%), field providers the least likely (56%), and upper-level management in between (67%).
In fact, respondents actually remain just as hopeful about EMS – perhaps even a bit more so – than they were before lockdowns and masks changed everything. Presented with the phrase “I am optimistic about the future of EMS,” 53% responded that they agreed or strongly agreed, a slight uptick since 2020. About a fifth of the 2,412 people who answered that question felt neutral, while the remaining 28% disagreed.
With the launch of the Centers for Medicaid & Medicare Services Emergency Triage, Treatment, and Transport (ET3) model, as well as the adjustments made by many organizations in response to the pandemic, treatment-in-place and telemedicine both gained momentum. Thus, it’s not surprising that only 5% of respondents stated treatment-in-place is not a service EMS should provide.
The support for telemedicine is not quite as strong, with only 41% of respondents agreeing to the idea that “telemedicine is the future of EMS.” It will be interesting to track that question as we move out of the pandemic response and wait to see whether payers and regulators support expansion of telemedicine or begin to revert back to pre-COVID policies and reimbursement rules.
In 2020, we asked whether the public understood the role of EMS professionals, and the answer was a pretty resounding “No.” This year, we posed a different question: Did respondents feel their organization effectively educates the public about what they do? The answer is still no, though not quite as overwhelmingly – possibly because management is willing to admit the public doesn’t understand EMS, but not willing to blame their organizations for not educating them.
Not only are EMS professionals skeptical that the public understands what they do, they also question whether their own organization’s employee assistance program (EAP) staff understand the job. Only 31% felt their EAP team understood the work of EMS clinicians, compared to 35% who did not.
EMS leaders have not been able to bridge the gap that several years of EMS Trend Report surveys show exists between management and field providers on issues related to safety. Perhaps it is simply the nature of our profession that field crews would not be as positive about their organization as leaders. This disconnect, though, is also a sign that providers do not feel empowered or included in decisions within the organization – a situation that, while common, is still a challenge that EMS organizations should strive to overcome.
The good news is that a majority of all respondents believe their organizations are taking patient safety seriously. The feeling is strongest among management and medical directors, among whom more than 85% agree that their organizations are prioritizing patient safety; that result drops to about 75% among field providers.
The gap is wider when it comes to clinician safety. Once again, 85% of leadership responded that it was a priority. This time, only 64% of ground field providers and 62% of flight paramedics and nurses agreed.
Perhaps most disturbing is that the gap widens when asked about prioritizing clinician mental health and fatigue, two issues that are known to impact the safety of not only the clinicians themselves, but also patients, EMS professionals’ families, and the general public.
These results are further illuminated by answers to the question, “If you could recommend to your chief one thing to improve provider safety at your agency, what would that be?” Fatigue and mental health were frequently mentioned. A sample of those responses include:
“Fatigue management program. This has been attempted, but gets push-back from ED Docs, Hospital Administration and others due to the huge amount of interfacility transfers on the agenda.”
“Ensuring that the personnel are not exhausted – which leads to patient care mistakes and many times careless errors, even placing the personnel themselves in danger.”
“Better support for mental health issues. In the fire departments across our county, there have been several Firefighter/EMS personnel suicides in the past few years, including one in our department. Yet nothing different is being done in our department to help those in need.”
“Better dispatch protocols for reduced lights and siren response. We use EMD, but EMD recommends too much lights and siren response.”
“We need more staff to ensure the mental and physical safety of our personnel. Too many providers are worked beyond their limits and staffing is too low to avoid accidents.
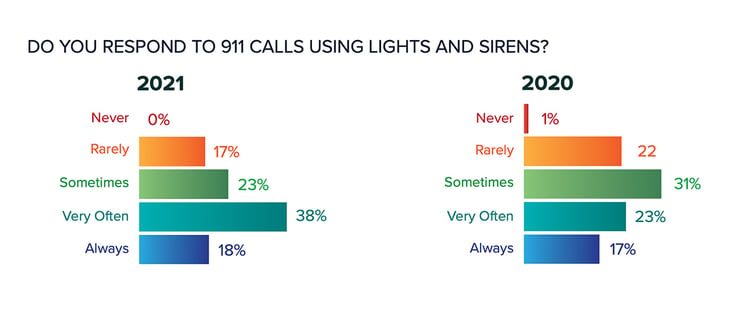
More than a third of all respondents feel that their organizations should reduce the use of lights and sirens. While that reflects awareness of the dangers of using lights and sirens, it also shows that despite that knowledge, we still have a long way to go. In fact, the 2021 Trend Report reflects a slight uptick in respondents who reported that their agencies use lights and sirens “always” and “very often” en route to incidents resulting from 911 calls.
The key will be bold leadership from EMS professionals at all levels throughout an organization who are willing to challenge one of the sacred cows of EMS and public safety, and take an evidence-based, safety-first approach to response and transport decisions about lights and sirens.
The topic of burnout among healthcare providers has received more attention thanks to the burdens of the COVID pandemic. That said, the EMS Trend Report indicates that while the pandemic highlighted a critical issue, it is one that has always been present and may not have been influenced by the pandemic as much as anecdotal reports would suggest. When asked to rate their own burnout symptoms, 2021 survey respondents reported the same level of burnout as the 2020 survey. Twelve percent reported constant symptoms of burnout and frequent frustration, or worse. Nearly one-fourth said they had “joy in work and no symptoms of burnout.” And the vast majority were somewhere in the middle, admitting to some stress or a symptom of burnout.
Just as COVID-19 does not appear to have had a significant impact on rates of self-reported burnout, it also doesn’t appear to have impacted people’s decisions to leave the profession. Just over half of survey respondents reported no plans to leave their employer, the same as in early 2020. And for those who do have plans, only 7% said it was related to COVID-19. Most cited wages and benefits or career advancement as reasons they were leaving their current employer, and the percentage who cite retirement as a reason has only ticked up slightly, from 27% to 31%.
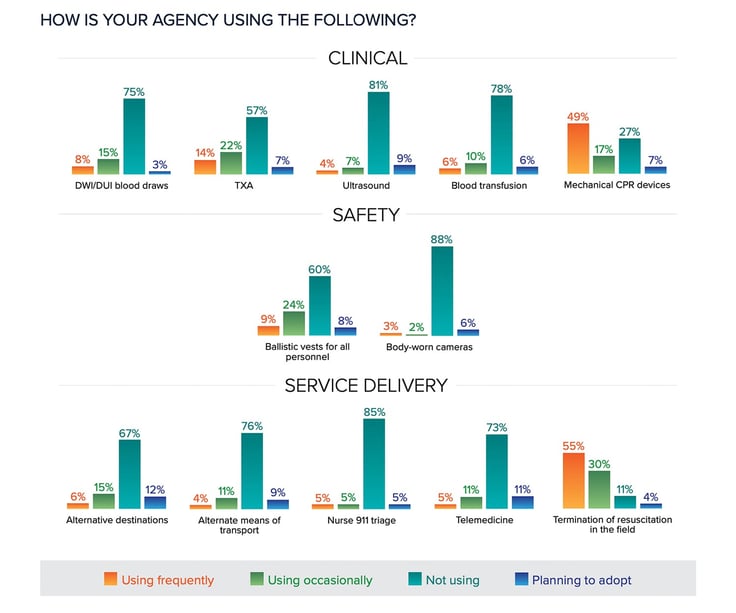
Ultrasound continues to gain a foothold in EMS, with a small increase in the percentage of people reporting their agency uses the technology in the field, from 7% to 11%, and another 9% reporting plans to adopt it soon. Mechanical CPR also remains popular, with nearly 70% reporting currently using mCPR devices, and another 7% planning to adopt them soon.
Not surprisingly, the use of telemedicine or video consults also increased, from 8% to 16%. What is surprising is that only an additional 11% said they were planning to adopt telemedicine technologies, despite the lessons learned during COVID-19 and the potential benefits to both patients and EMS systems.
Likewise, the use of nurse triage of 911 calls and alternative destination protocols seem to be increasing in popularity, but still less than one might expect after COVID. That said, the ET3 program, along with lobbying to make temporary pandemic measures more permanent, may change how EMS is reimbursed for such activities, making these topics ones to keep our eyes on in future years.
Last year, we saw that just prior to the onset of the most significant global pandemic in a hundred years, EMS professionals had little confidence in their organization’s ability to respond to such an event. Only 3% responded that their agency was “extremely well prepared,” with 15% responding “well prepared” and 22% responding “not prepared at all.” Thanks to having now lived through that pandemic, the confidence level among EMS has actually increased significantly, with half of all respondents responding their organizations are either extremely well prepared or well prepared – and only 6% continuing to argue that their organizations are not ready at all.
That shift appears to have carried over to other types of major events as well, with respondents more confident that their organizations are prepared for natural disasters and active shooter incidents and, to a lesser degree, even cyberattacks – although that positive shift was not nearly large enough to change the overall view that their organizations are not ready at all for an attack on their technology systems.
We’ve heard the clichés throughout 2020 and into 2021: “A year unlike any other.” The results of the 2021 Trend Report might indicate, though, that while COVID-19 brought unprecedented challenges to each of us, at work and at home, the profession came through largely intact and as strong as before. Our interpretation though is a bit different. What we see is that, as they have for decades, EMS caregivers across the nation stepped up to the challenge of the pandemic. And that when the pandemic fades, the same critical issues that threaten EMS agencies’ very existence and the health and happiness of their personnel remain.
The real test will come next year, once we’ve had more time to recover and, perhaps, reinvigorate our efforts to improve. The 2021 EMS Trend Report shows that the greatest public health challenge in generations did not cripple the profession. Let’s hope the 2022 survey shows that we emerged from that event inspired and ready to tackle the problems before us and make EMS better for clinicians, communities and patients.
About the Author
Anthony Minge, EdD, is a senior partner at Fitch & Associates. He has more than two decades of leadership, revenue cycle management, compliance and healthcare business operations experience. Prior to joining the firm, he was the business manager for Northwest MedStar in Spokane, Washington.
Pulsara is helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...