Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

EDITOR'S NOTE: Special thanks to our guest blogger, Bob Sullivan. Bob Sullivan, MS, NRP, is a paramedic instructor at Delaware Technical Community College. He has been in EMS since 1999, and has worked as a paramedic in private, fire-based, volunteer, and municipal EMS services, and is an ally to Pulsara. Contact Bob at his blog, The EMS Patient Perspective. Enjoy!
__
EMTs and paramedics play a crucial role in rapid detection, treatment, and transport of STEMI1 patients to the most appropriate hospital. Here are the top 10 things you need to know about STEMI to save lives:
The longer it takes for a patient to receive reperfusion therapy, the higher the risk of death or a reduced quality of life. When a coronary artery is completely blocked, irreversible damage to heart muscle occurs until reperfusion. Opening the blood vessel and restoring blood flow is done in the hospital with emergency angioplasty or thrombolytic medications.
Angioplasty, also known as percutaneous coronary intervention (PCI) is the most effective method of reperfusion.
However, PCI is not available at every hospital. STEMI patients who arrive at a non-PCI center must be transferred or given thrombolytic medications, which are less effective and have more side effects. STEMI patients should be taken to a PCI center if transport time is less than 90 minutes, even if other hospitals are closer.
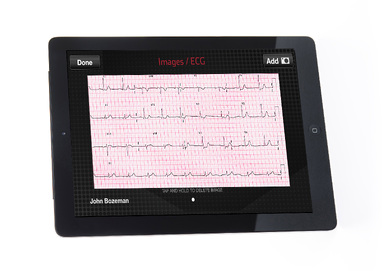
STEMI care starts with recognition, which requires capturing a 12-lead ECG as early as possible on any patient with a possible ACS.
Perform a 12-lead ECG with the first set of vital signs on any patient with ONE of these symptoms: chest discomfort (often described as a heaviness or pressure that may radiate into the left arm, jaw or shoulder), shortness of breath, nausea, vomiting, weakness, or diaphoresis. STEMIs can lurk in unsuspecting places, especially in elderly, female, and diabetic patients. They also evolve and may not be on an initial ECG, so keep the leads connected and perform additional 12-leads during transport.
The 12-lead ECG primarily views the septum and left ventricle of the heart, where most STEMIs occur. But a standard 12-lead may not detect ST elevation affecting the right or posterior walls of the heart. View those regions by moving one lead to the right side of the chest, and two leads underneath the shoulder blades after the initial 12-lead is complete. Alternatively, you can check the posterior by looking at the anterior leads.
15-leads increase the sensitivity of STEMI detection and localizes the infarct, which guides treatment.
Prehospital 12-lead ECGs have been shown to reduce the time to reperfusion in hospitals. A STEMI alert may be activated based on a transmitted ECG to the emergency department or a paramedic’s interpretation of the 12-lead and calling in a STEMI alert.
At PCI centers, the cath lab must be prepared, staff called in during off-hours, and elective procedures delayed. When these tasks are done prior to arrival, EMS may bypass the ED with STEMI patients and go directly to the cath lab for faster coronary reperfusion. You will need to notify the hospital early so they can marshal the resources they’ll need.
After time to reperfusion, the next most important interval is time to aspirin. Aspirin inhibits platelet aggregation that would make the clot larger, thus slowing down damage to the heart muscle. Chewing and ingesting 160-320 mg of aspirin is a pre-arrival instruction in many 911 call centers and BLS protocols.
One long-standing treatment that has fallen out of favor is routine oxygen administration. High flow oxygen has been shown to cause vasoconstriction, which increases infarct size. Only administer oxygen to ACS patients who are short of breath and only enough to titrate the pulse-ox reading to 94%.
When the heart muscle is dying from an infarct, easing its workload may slow infarct progression. Nitroglycerine, available in sublingual tabs, spray, paste, or an intravenous infusion, accomplishes this through vasodilation, which decreases preload and afterload.
A damaged right ventricle can reduce preload to the left ventricle, which could be made worse if nitroglycerine is administered. When a right-side STEMI is identified, the treatment of choice is a fluid bolus to increase contractility. Use nitroglycerine with caution, if at all, with a known right-side infarction.
Other causes of ST elevation include pericarditis, benign early repolarization, bundle branch blocks, hypertrophy, and pacemakers. Be aware of these subtle differences in ECG interpretation to prevent an inappropriate STEMI activation. While a certain degree of over triage to the cath lab is acceptable, false activations drain hospital resources that could be utilized elsewhere.
An EMS performance benchmark paper states that for every fifteen STEMI patients who receive a prehospital ECG, aspirin, and transport to a PCI facility, one stroke, second MI, or death is prevented2. Successful STEMI systems of care require cooperation from EMS, multiple hospitals, and departments within hospitals.
To provide the best care to the STEMI patient, EMS services need to get the right patients to the right facilities, and a clear path to reperfusion must be in place at those facilities. Early activation of the receiving hospital is critical. Hospitals must mobilize resources. Spending seconds to notify the hospital early saves muscle, morbidity and lives.
1. ST-elevation myocardial infarction, known as STEMI, is an acute coronary syndrome (ACS) that is diagnosed with a 12-lead ECG. When the ST segment in at least two leads covering the same area of the heart is elevated 1 mm or more above baseline and a patient has symptoms of an ACS, this indicates that heart muscle is dying from a blocked artery. STEMI is usually caused by a plaque rupturing in a coronary artery forming a thrombus, which blocks blood supply to cardiac muscle.
2. Myers JB, Slovis CM, Eckstein M, et al. Evidence based performance measures for emergency medical services systems: a model for expanded EMS benchmarking. Prehosp Emerg Care, 2008; 12: 141–51.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...