Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
6 min read
 Team Pulsara
:
Mar 22, 2021
Team Pulsara
:
Mar 22, 2021

EDITOR'S NOTE: Special thanks to Kinsie Clarkson (Pulsara's Product Marketing Specialist, 2020-2025) for writing today's blog post. You can connect with her on LinkedIn.
__
When COVID-19 spread globally last March, New Zealand reacted quickly. In fact, their shut down was so effective that they were able to have a much shorter period of quarantine than most other countries. They quickly mobilized technology to help pivot and shift toward virtual appointments, utilizing telehealth to help manage patients’ needs.
Though brief, this period still has New Zealand experts looking to the future of health—a future which might just lie in the more strategic use of infrastructure and technology.
In a recent interview with Newsroom, leading authorities and experts shared their belief that the best path forward lies not in building newer, bigger facilities, but in new infrastructure and technological solutions that are tailored to the needs of communities.
Over the course of the pandemic, technology has proved its effectiveness for use in virtual appointments—decreasing pressure on New Zealand's brick-and-mortar facilities. Prior to the pandemic, about 5% of New Zealand’s health consultations were conducted remotely. During lockdown, that number increased to around 75%, with involvement from around 5000 practices nationwide. Other new systems also quickly became popular. Previously, prescriptions required a physical signature for most patients going to a pharmacy. In April and May of 2020, about 500 practices activated with the national electronic prescribing system.
Ranjna Patel, a director and founder of Tamaki Health, one of the country's largest primary care providers, discussed how during the lockdown, her facility converted to mostly virtual consultations. "It was phenomenal. We realised that's what people needed," she said.
According to Dr. Ruth Large, chair of the National Telehealth Leadership Group and an emergency physician at Waikato DHB, New Zealand achieved about five years of telehealth activity in the March-to-May period of New Zealand’s lockdowns. During that time, they observed several other benefits: Non-attendance rates at appointments were much smaller; patients did not need to travel to their appointments, saving a great deal of time; health providers could remain in their hometown; and overall, there was evidence of less need for brick and mortar facilities.

Physically attending doctors’ appointments regularly costs New Zealanders a great deal of time. The Simpson review of the health and disability sector, overseen by Heather Simpson, the former chief of staff to Prime Minister Helen Clark, suggests that at any given hour of every weekday, around 2000 New Zealanders are stuck waiting in a physical queue for an appointment somewhere in the system. "Assuming there is three hours of time per visit (which is conservative)," the report says, "this amounts to 11 million hours of time per year that patients are just travelling or waiting. The magnitude of this time cost alone demonstrates why future service planning should prioritise reducing travel and time costs by offering virtual options where possible."
Additionally, New Zealand’s current co-payment system results in most patients choosing to go to the Emergency Department, which is free, instead of visiting a primary care provider, who charges. The majority of traffic then ends up at the ED, even when a GP is perhaps more suited to caring for the patient’s ailment. In the 2019/2020 year, 13.3% of adults said they could not visit a GP due to cost. Though there are no stats on whether that population chose to go to the ED instead, emergency departments are struggling under the volume of incoming patients, making it a likely factor. “It's not the main reason people turn up to ED, but it is still a pretty big reason," shared Associate Professor of the University of Auckland's School of Population Health, Tim Tenbensel. He believes that providing more services in the community, especially services with a more preventive focus, could help with the issue. "If not addressed, we are going to continue to have hospitals used in ways that may not be ideal."
With the discoveries made during lockdown in 2020, New Zealand is working toward solutions to remove barriers for telehealth.
First steps include improving the quality of internet service, to facilitate more stable video interactions. “With telehealth, it's not okay to say the internet is slow for video," said Dr. Large. "It's a must-have for rural communities and those who are disadvantaged." Once those capabilities are in place, health services could expand beyond virtual appointments to include diagnosis. "Very few of your final diagnostic bits come from the 'laying-on of hands'. Most come from talking to your patient,” said Dr. Large.
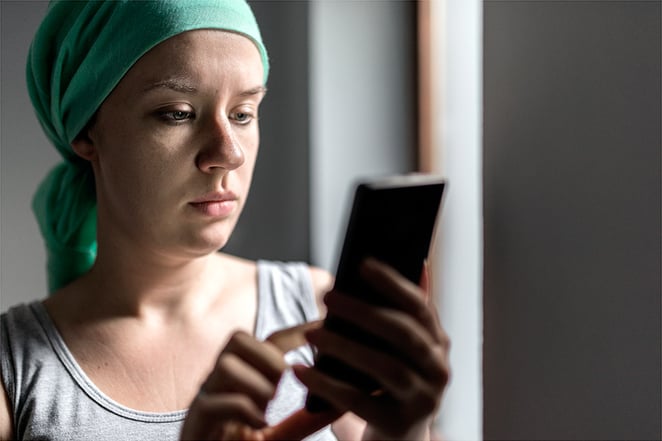
Though 81% of New Zealanders own smartphones, affording the data to use them can be a different story. As such, the health ministry, the Department of Internal Affairs, and the country's telecommunications providers are working together to pilot 'zero-rated' data to consumers for certain websites. This way, New Zealanders can gain access to certain healthcare online services without having to pay extra for them. The Simpson report advocated a permanent—and expanded—use of zero-rated data in New Zealand, stating that “Approaches like this have shown a considerable impact, as well as return on investment overseas.”
Experts believe that moving forward, infrastructure must be the main emphasis—and, even more importantly, an emphasis on making that infrastructure sustainable for the future. Rather than centering only on improving hospitals, there needs to be an equal focus on moving health into the community—and that means investing in technology that can do just that.
Richard MacGeorge, a member of the New Zealand Infrastructure Commission, Te Waihanga, believes that there is a need to anticipate the direction of health before moving forward. "There's an assumption that health has to be carried out in a healthcare facility,” he said. “But what is the role of the hospital going to be, say, in 2050? Is the current model going to be continued for the next 20 or 30 years or is it likely there will be some fundamental change?"
Kelvin Keh, of UniServices at the University of Auckland, agrees. "We need a clear idea first of how we want to look after our population in the next 50 years, because the investment in infrastructure has to be secondary to that answer,” he said. "Essentially the healthcare infrastructure of today will not be able to cope with the burden in 50 years' time, given the increased lifespan of our populations and associated chronic conditions. I expect we will see more forms of personalisation where services are tailored to particular demographics to enable better outcomes. This will likely be a mix of services within clinical settings, at home and in the community."
And when it comes to updating existing facilities, technology will play a vital role. The Simpson report noted: "This level of investment may be daunting, but it also presents an opportunity. The health and disability system could look at replacing ageing facilities with ones designed and planned for the future. New facilities can use technology to support new ways of delivering specialist services, embrace the shift of services closer to home, and be a great place for the future health workforce to work in."
Ranjna Patel believes that the time is right to think again about big infrastructure spends on hospitals, but advocates for a smarter approach to allocation. "The thinking has got to be: 'Who has what competencies?' You cannot be building bigger hospitals when there are things they [patients] do not need to go to hospital for."

After the COVID-19 pandemic, experts say they see promise for the future. The systems will need to maintain the innovative momentum generated by the pandemic; however, barriers were broken, and they are optimistic that things will change.
According to Tenbensel, significant change has been discussed for awhile, but has never seen much follow-through—until now. "For 20 to 30 years, all governments and all health systems have had an absolute mantra that we need to move things out of the hospital and into the community. But in that time, we've not seen any real movement in any high-income country.... There might be a tipping point that we reach in the future, but it is hard to see that right around the corner."
Ranjna Patel feels that the pandemic has made bureaucrats more willing to consider new and different approaches—which has not been the case in the past. A primary example is the recently allocated funding for telehealth. Last March, the government dedicated $20 million to improve video conferencing and telehealth consultations. In September, they added $7.1 million more for DHBs and $3.4 million for GPs. What is needed, Patel says, is follow-through. For example, the funding increase for mental health in primary care that was approved well over a year ago only became accessible to providers a few months ago.
Simon Royal, chief executive of the National Hauora Coalition, a Māori-led Primary Health Organisation, believes that New Zealand’s care system can only move forward with a stronger consideration for equity and better inclusion of Māori, as well as adopting the Māori’s more holistic view of health. Pouring more money into the same old structure, he says, is not the solution. "Right now, our systems in that regard are quite archaic, in the way they deal with Māori. They are simply not fit-for-purpose, both at a primary care level and secondary and tertiary services. If you are talking seriously about addressing inequality and reducing downstream fiscal costs, this [the new models] is the stuff you need to invest in."
Though many things will need to happen to create lasting change, New Zealand's experts are optimistic that last year's lockdown could just be the impetus the country needs.
Thinking about trying telehealth, but aren’t sure where to start? The right telehealth platform should be able to scale up or down to meet your needs. Check out Quadruple Aim: How One Telehealth Platform Is Changing the Game to learn more.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...