Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Inoculate EMS leaders with the skills necessary to effectively lead our caregivers and organizations
Editor's Note: On August 11th, EMS1, Fitch & Associates, and the National EMS Management Association released their fourth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is written by Anthony Minge, Ed.D., a senior partner at Fitch & Associates.
Hopefully, we are nearing the end of one of the worst healthcare crises in modern times. At the time of this writing, there have been over 187 million known cases of COVID-19 worldwide and over 4 million deaths, in excess of 600,000 deaths in the U.S. alone. The COVID-19 pandemic has impacted and been a drain on almost every single aspect of humanity, in many instances, devastatingly and critically. The effects on our economy, healthcare system, and society will continue to be felt for years to come. EMS and public safety have literally been on the front lines since the beginning and the impacts have most certainly not been positive.
 This year’s EMS Trend Report survey respondents rated provider safety as the No. 3 concern behind mental health, which ranked seventh and fifth respectively in the 2020 Report. This comes as no surprise, given the associated concerns this coronavirus has given rise to. While public safety concerns could also be attributed to the rise in riots and social unrest, there are pandemic-related factors that undoubtedly contributed to each of these critical issues rising in the rankings. Shortages of PPE; increased potential for exposure; fears of spreading the virus to family and friends; and seeing patients, peers, and loved ones lost at the hands of this pandemic, as well as ongoing effects that negatively impact the organization, have all been brought on by and can be directly linked to COVID-19.
This year’s EMS Trend Report survey respondents rated provider safety as the No. 3 concern behind mental health, which ranked seventh and fifth respectively in the 2020 Report. This comes as no surprise, given the associated concerns this coronavirus has given rise to. While public safety concerns could also be attributed to the rise in riots and social unrest, there are pandemic-related factors that undoubtedly contributed to each of these critical issues rising in the rankings. Shortages of PPE; increased potential for exposure; fears of spreading the virus to family and friends; and seeing patients, peers, and loved ones lost at the hands of this pandemic, as well as ongoing effects that negatively impact the organization, have all been brought on by and can be directly linked to COVID-19.
Oddly enough, pandemic recovery was at the bottom of the list of concerns. This is because healthcare professionals and caregivers in this industry have faith in science and the system, and know undoubtedly, we will get through this, just like we have other epidemics, disasters, and catastrophes.
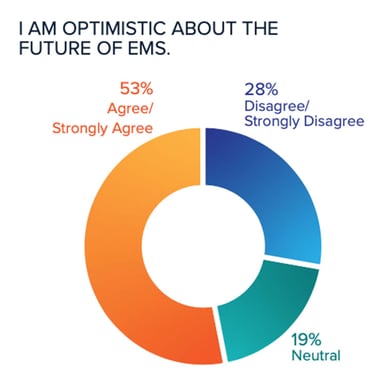
Refreshingly, optimism is on the rise. With proven resiliency and ability, EMS continually meets and overcomes the challenges faced, provided they have the most important dynamic: high-quality leadership.
Poor or toxic leadership can be as harmful to the organization as a whole – and I will venture to say more so – as the ill-effects suffered during the pandemic. The consequences of either can be eerily similar in nature and outcome. For example, shortages, fears, contamination, and losses are common undesirable effects associated with both pandemics and poorly led organizations. Allow me to further explain how poor leadership results in these and other unfavorable outcomes.
Shortages. Poor leadership most always results in a variety of shortages that lead to other deficiencies, and ultimately become detrimental to the ability to complete the mission and even the stability and sustainability of the organization. Examples of shortages that can result from poor leadership include:
Time. Employee issues and concerns are dismissed or not appropriately responded to in a timely manner.
Resources. Materials, supplies, equipment, contracts, education, and even personnel to perform the mission are not readily available. Failure to procure and maintain consistently adequate resource levels has a negative impact across the organization.
Structure and processes. A lack of effective planning or process development results in reactionary decision-making, leading to a failure to promptly and appropriately respond to critical issues and, oftentimes, even routine issues resulting in a “nothing gets done” culture.
Confidence. Employees, referrals, receiving entities, patients and communities can develop a lack of confidence in the abilities of the agency.
Exposure. Poor leadership exposes the system to increased scrutiny from executive management, the medical community, contracts, patients, payors, and the community.
Fear. Anxiety, dread, apprehension, and distress are commonly associated signs, symptoms, and results of poor leadership. 
Contamination. Poor leaders’ unhealthy attitudes spread throughout the organization, infecting others, often resulting in a lack of motivation to do good work and even resentment of the organization, for the job, and, in the worst-case scenarios, the profession as a whole.
Loss. Lost business, employees, and even lives can occur through a decline in business volume or cancellation of contracts due to poor service performance:
Quality of work and customer service suffers.
Referral sources, contracts, and even patients may seek out alternate means of transportation or turn to competitors when available.
Inferior leadership skills are often directly linked to poor financial management, resulting in loss of revenue impacting the ability to provide the necessary resources for top-quality service.
Employee retention continues to be a top concern in the EMS industry. Poor leadership only exacerbates the issue.
And as we are well aware, there is a mental strain associated with the public health industry, and far too often, this results in the loss of loved ones through failed relationships and even worse, suicide. Ninety-four percent of this year’s respondents noted provider mental health is having an impact on the industry. Poor leadership fails to give appropriate attention to, or often even recognize and appreciate the magnitude of this significant issue in the EMS industry.

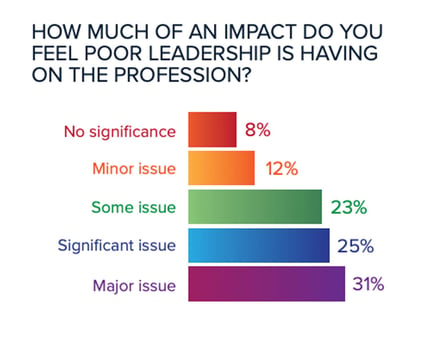
The harsh reality is that there is a leadership issue in EMS. Almost 80% of survey respondents felt that poor leadership is having some impact on the profession, with more than 50% of all participants ranking it as significant or major. While this is a perceived risk, identified through a survey, it cannot be ignored. As the saying goes, perception is reality. Numerous comments in the survey’s open text responses referenced leadership. Most of these were negative in nature, stating among other things, a need for better, higher quality, attentive leadership, or a lack of, or even “no” leadership. In many instances, terms such as “poor,” “ineffective,” “inadequate” and even “toxic,” were used in describing leadership within the respondents’ EMS organizations.
Poor leadership can certainly cause more long-term damage to an EMS organization than the pandemic. The people of this industry have proven their resiliency time and again when faced with crisis. They have risen to the challenges presented by forces external to their organizations. An infection brought on by poor leadership will spread rampantly, causing damage that may take months or years to overcome. In some, worst-case scenarios, it may even result in the death of the company.
EMS agencies must be proactive and regularly assess the health of the organization. If the ill-effects of poor leadership appear to be infecting the agency, action must be taken immediately. We do not have the luxury of closing shop in hopes it will just go away. Providing our supervisors, managers, directors, chiefs and others in positions of authority with quality training to enhance and support the skills necessary to effectively lead our caregivers and organizations will hopefully serve to ward off the ill-effects of poor leadership.
Download the full 2021 EMS Trend Report
About the Author
Anthony Minge, Ed.D., is a senior partner at Fitch & Associates. He has more than two decades of leadership, revenue cycle management, compliance and healthcare business operations experience. Prior to joining the firm, he was the business manager for Northwest MedStar in Spokane, Washington.
Pulsara is helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...