Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
4 min read
 James Woodson, MD
:
Jul 24, 2020
James Woodson, MD
:
Jul 24, 2020
![Finding a Next-Generation Telehealth Plan of Action for Your Hospital [Part 1]](https://www.pulsara.com/hubfs/provider-to-patient-video-1.jpg)
This 5-part blog series is based on the webinar “The Next-Gen Communication and Telehealth Plan of Action for Your Hospital.” Watch the corresponding section of the webinar below, or listen to the full webinar here.
Telehealth and telemedicine have gone through dramatic changes over the last four months, far more than many of us dreamed possible. Regulations and reimbursement are evolving rapidly, which has opened up the door to many new opportunities for using telehealth. Telehealth is helping us improve both the quality and the value of the care that we deliver to our communities.
However, all this change will almost certainly have wide-reaching implications for your health system, especially in the acute care space. Over the next five posts in this series, we’ll discuss the rapidly shifting landscapes of telehealth regulations and reimbursement and how you can navigate them. We’ll also dive into some of the questions surrounding how to best leverage telehealth in the acute care space.
We can't talk about telehealth without talking about COVID-19. COVID is the reason telehealth is growing and changing at such a rapid rate. We find ourselves faced with so little—as well as so much—information and data at the same time. In addition, we're undergoing change at such a rapid rate that many are left feeling discombobulated, and often don't really know how to react to the situation or what to do next. To simplify, let’s break down where we are into three phases.
Phase one encompasses the initial response: we all did what we had to. Back in March, we did our best to handle the situation and leveraged the tools that we had available to us. Now, we're starting to enter into phase two. I believe Winston Churchill's famous quote applies to this exact moment in time: "Now is not the end. It's not even the beginning of the end. But it is, perhaps, the end of the beginning." We have reached the end of the beginning of this pandemic. We have moved past the initial reactionary phase, and are now thinking about how to navigate the road ahead. Many of us are now reflecting back and evaluating what we've done, how we responded, and how we need to prepare for what comes next.
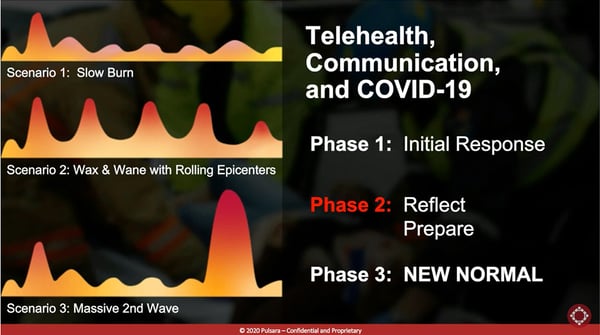
And that’s part of the challenge: We don't know what comes next. Is this going to be a slow burn? Are we going to have rolling epicenters, with waxing and waning? Are we going to have a large second wave? We don't know, but we do know that now is the time to reflect and prepare for what's next.
Systems of care highlight the fact that we must unite, and that we're all in this together. Inter-organization communication with fax, phone, and radio is obviously no longer acceptable. I personally believe that how we work with others will be the defining characteristic of our response, and I believe telehealth will be a key driver of that. As we take a step back and reflect on where we've been and what's happened, part of reflecting is evaluating this initial response: what worked, and what didn't. The answers will be different for each individual and organization, but honestly evaluating and taking steps to adjust accordingly will be crucial in moving forward.
 There is one common theme that we should all be reflecting on, though, and that is the vast realm of unexplored potential in telehealth. Telehealth is rapidly evolving and will continue to play a major part in the shifting landscape of healthcare communication. CMS Administrator Seema Verma's now-famous quote sums it up well: "I think the genie's out of the bottle on this one. I think it's fair to say that the advent of telehealth has been just completely accelerated, that it’s taken this crisis to push us to a new frontier, but there's absolutely no going back." We have crammed decades of progress into three months.
There is one common theme that we should all be reflecting on, though, and that is the vast realm of unexplored potential in telehealth. Telehealth is rapidly evolving and will continue to play a major part in the shifting landscape of healthcare communication. CMS Administrator Seema Verma's now-famous quote sums it up well: "I think the genie's out of the bottle on this one. I think it's fair to say that the advent of telehealth has been just completely accelerated, that it’s taken this crisis to push us to a new frontier, but there's absolutely no going back." We have crammed decades of progress into three months.
Now that the red tape has been cut and telehealth is becoming increasingly accessible, the endless possibilities have also sparked a number of questions:
Over the next few posts, we will explore some of these questions. The question that needs to be tackled first, however, is: how permanent are the restriction changes going to be?
 And though suspending many government restrictions on telehealth was meant to be a temporary pandemic mitigation measure, it’s becoming clear that even once the restrictions are reinstated, things will never be the same. Recently the U.S. Committee on Health, Education, Labor, and Pensions met to discuss the thirty-one temporary federal policy changes, and decide which should continue on after the pandemic. Two of the modifications that they believe should be permanent include relaxation of the patient’s location and the originating site rule, and expansion of reimbursement services, both in terms of types of encounters and the eligible providers. Based on the discussion, it’s highly likely that those changes will at some point be made permanent to some degree.
And though suspending many government restrictions on telehealth was meant to be a temporary pandemic mitigation measure, it’s becoming clear that even once the restrictions are reinstated, things will never be the same. Recently the U.S. Committee on Health, Education, Labor, and Pensions met to discuss the thirty-one temporary federal policy changes, and decide which should continue on after the pandemic. Two of the modifications that they believe should be permanent include relaxation of the patient’s location and the originating site rule, and expansion of reimbursement services, both in terms of types of encounters and the eligible providers. Based on the discussion, it’s highly likely that those changes will at some point be made permanent to some degree.
There are, however, certain things that we know will be discontinued: the relaxation of the privacy and security standards, for instance. While necessity drove many to adopt non-HIPAA compliant solutions in an effort to put a workable solution in place to help survive the crisis, those solutions will only continue to work on a limited timeframe.
We’ll come back to the implications of suspended security restrictions more in the third post in this series. In part 2, Pulsara’s Senior Vice President of Product, Tim Hakamaki, will take a deeper look into the past, present, and future of telehealth.
To learn more about creating a next-generation communication and telehealth plan for your hospital, listen to the full webinar here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...