Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
2 min read
 Hannah Ostrem
:
Aug 30, 2019
Hannah Ostrem
:
Aug 30, 2019
Editor's Update: As reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Please be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
__
As the scope of practice for first responders expands and they become increasingly empowered to treat patients within the community, incentives like the Centers for Medicare and Medicaid Services (CMS)'s Emergency Triage, Treat, and Transport (ET3) model have emerged.
According to the CMS, "Currently, Medicare regulations only allow payment for emergency ground ambulance services when individuals are transported to hospitals, critical access hospitals, skilled nursing facilities, and dialysis centers." As a result, most patients who call 911 are therefore transported to one of these destinations, even when their conditions could be treated at home or another non-emergency care facility. This is where ET3 comes in.
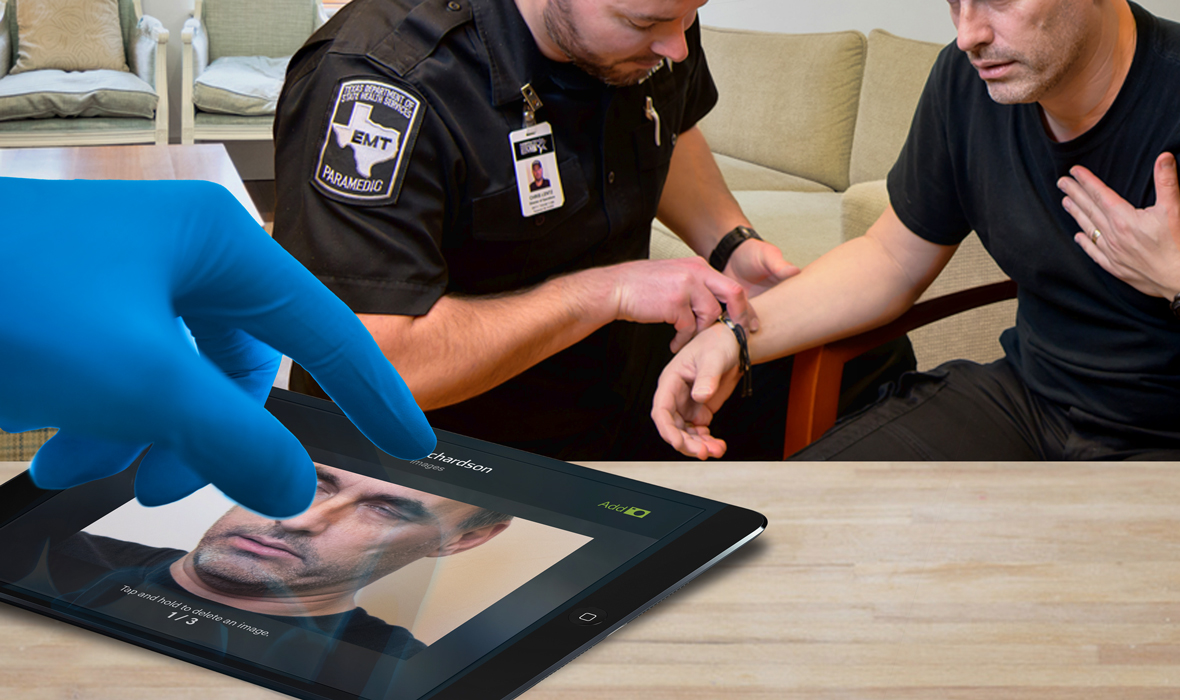
ET3 is an EMS reimbursement program introduced by CMS to empower first responders to make care decisions in a broader scope of practice, taking into consideration the patient's care goals and determining the most appropriate treatment step. Those next steps can include treating the patient in their home in conjunction with a qualified care provider via telemedicine (in a CP scenario), transportation to an out-of-hospital facility, such as a primary care facility, or transportation to the most appropriate emergency department (ED). Ultimately, ET3 aims to reduce unnecessary ED transports, thereby reducing costs and improving quality of care.
It’s important to note that if an agency chooses to treat-in-place (also note that this is not required — programs only need to establish alternative transport destinations), ET3 requires “multimedia communications equipment that includes, at a minimum, audio and video equipment permitting two-way, real-time interactive communication between the patient and distant site physician or practitioner. Telephone, facsimile machines, and electronic mail systems do not meet the definition of interactive telecommunications systems.”
Because ET3 is designed to reduce the burden on EDs, it highly encourages the use of Community Paramedicine programs. Some forward thinking health systems, such as Northwell Health Center for EMS, have already been practicing and conducting research about community paramedicine programs, which are a natural fit for the ET3 model. Lessons learned from systems like these can and should be applied to those looking to participate in the initial ET3 programs. Some of those lessons were nicely summarized in the EMS World article, It Takes a Team of Teams to Transform Healthcare.
Additional published research and resources on CP include:
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...