Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
6 min read
 Team Pulsara
:
Jul 24, 2019
Team Pulsara
:
Jul 24, 2019
![EMS Providers and Leaders Share their Perception of the State of EMS [EMS1 2019 EMS Trend Report Part 1]](https://www.pulsara.com/hubfs/medic-ems-radio-report-1.jpg)
EDITOR'S NOTE: Earlier this month, EMS1, Fitch & Associates, and the National EMS Management Association released their fourth annual EMS Trend Report, proudly sponsored by Pulsara. Read, ponder, and share the following information brought to you by the most prestigious thought leaders in EMS.
By Roxanne Shanks, MBA, and Jay Fitch, PhD
This year began with reasons to feel hopeful about the future of EMS. In February, the Secretary of Health and Human Services announced a pilot program to reimburse ambulance providers for transport to alternative destinations and for treating but not transporting – a trial run of what would be the most significant change in decades in how Medicare pays for EMS care. While the details have yet to be revealed, the Emergency Triage, Treat and Transport model (ET3) has energized many in the profession who hope it is a significant step toward recognizing the true value paramedics and EMTs can bring to individuals and communities.
The announcement came on the heels of the release of EMS Agenda 2050, a vision for the future of EMS created by members of the profession. It describes a people-centered EMS system, one where clinicians and agencies are incentivized to do the right thing for the patient, take advantage of new technologies and other innovations, and focus on evidence- based interventions. Developed through a two-year, collaborative process, EMS Agenda 2050 is intended to unite our profession behind common goals.
As we see in these pages, our fourth annual EMS Trend Report, a wide range of opinions still proliferates through EMS, with some clear divisions on topics ranging from education, to what we should call ourselves.
The online survey was conducted in early 2019. Responses were received from nearly 3,000 individuals from a diverse representation of communities, system models and years of EMS experience.
Survey questions were developed by Fitch & Associates in collaboration with the EMS1 Editorial Advisory Board and National EMS Management Association. A cross section of educators, EMS providers and EMS leaders vetted the questions prior to public release.
The Trend Report survey was completed by EMS professionals from all 50 states and the District of Columbia, as well as several in Canada and serving in the military overseas. They serve urban, suburban and rural communities in different service models and different roles.
In last year’s report, recruitment and retention stood out as the clear top concerns of EMS professionals, from field providers to chiefs. This year is no different, as the workforce continues to be the most critical issue for the profession according to survey respondents, followed by reimbursement and provider mental health.
For the first time, respondents were also asked why they thought people were leaving their agencies, as well as whether they planned on moving on from their current employer. Wages and benefits topped the list of reasons people were moving on to new opportunities, especially among for-profit ambulance services. Career advancement and career change also showed up prominently on the list.
One way to improve both recruitment and retention is to try to better understand what EMS clinicians are looking for and why they stay in the job. Recognizing that those answers might change over the course of a career could be key to recruiting the right people and keeping them in the profession. In this year’s survey, we asked what factors respondents found most satisfying about working in EMS and found the answers varied depending on their levels of experience. While patient interaction and intellectual stimulation ranked at the top nearly across the board, the number of people who chose “adrenaline rush” was much higher in those in their first five years (11%) and five to 10 years (7%) than those with more experience.
More than a quarter of private, for-profit respondents planned to leave their current employer in the next zero to 12 months. Less than 10% of fire or public utility respondents planned to leave their employer in their first year.
Diving deeper into this issue will be critical for the profession. Are people who get into the job because of the adrenaline rush less likely to stay? Or are they just more likely to change their priorities as they’re in the career longer? It’s important to recognize how these factors could influence both recruitment and retention.
This year’s survey captured the thoughts of more than 130 EMS medical directors. As leaders of EMS organizations with a unique connection to both EMS and the healthcare system, medical directors will be key to the evolution of EMS and the paramedicine profession.
Unfortunately, the number of field providers who agreed with the statement that their medical director was “very engaged” with them remained this year at only 47%. Another sign that medical directors might not be as engaged in the overall operations and management of their organization: Nearly a quarter of medical directors were not sure if their organization’s budget had increased or decreased over the previous year.
Medical directors’ opinions on some of the more controversial topics in EMS today were similar to those of their colleagues throughout the ranks of EMS, but with some notable differences. Overall, only 15% of respondents feel a bachelor’s degree should be required for paramedics; among physicians and medical directors, though, 24% want to see that as a requirement.
Medical directors also overwhelmingly support the term “emergency medical services” to describe the profession, rather than alternatives, such as mobile integrated healthcare or paramedicine. While the majority of survey respondents leaned in that direction, paramedicine earned higher support among field providers and managers than medical directors. These preferences could stem from many reasons, including the recent creation of an official EMS subspecialty of medicine. If proponents of the term paramedicine hope to create a professional identity for EMS clinicians, gaining the support of their physician colleagues will likely be an important step.
The medical directors surveyed are a hopeful group, though, and feel more enthusiastic about what’s in store for EMS than any of their counterparts. Nearly 80% of the physicians who responded said they agreed with the statement, “I am optimistic about the future of EMS,” while only 54% of field providers and 64% of managers and chiefs felt the same.
Despite the publicity around active shooter incidents, the seemingly ever-increasing threat of infectious disease and frequent major natural disasters, respondents continue to feel largely unprepared to respond to such catastrophic events. For example, 16% of respondents in 2018 and 2019 are “not at all prepared” for an active shooter incident.
Point-of-care testing, ECMO in the field, IV acetaminophen and impedance threshold device continue to have low adoption across respondents. Just 3% of respondents report nurse triage of 911 calls and 8% report telemedicine adoption, though we may expect these figures to change in the years ahead as ET3 emphasizes triage.
Across healthcare, provider burnout is receiving critical attention. Surveys of physicians have revealed high levels of burnout, with concerns that the declining mental and physical health of the workforce will lead to shortages of experienced clinicians down the road.
Overall, 12% of those surveyed reported high levels of burnout, with the highest numbers coming among field supervisors and respondents whose primary EMS role is with a private, non-profit service. Members of the fire service had the lowest levels, with more than a quarter saying they have no symptoms.
Despite relatively low numbers of self-reported burnout, provider mental health continues to be a concern of EMS professionals, with 62% stating it is having a significant or major impact on the profession. As in past years, there continues to be a disconnect between field providers and leadership as to whether they are addressing the problem. Among field providers, only 28% agree (a slight decrease from the 33% in 2018) that their service is making provider mental health a priority, compared to 59% of managers and chiefs, and 46% of medical directors. Members of public agencies (fire departments as well as third-service EMS departments) tended to think their organizations were tackling the issue more than those working for private companies.
As far as actual actions regarding patient and provider safety, perhaps nothing is more telling than whether we as a profession are addressing two known issues:
The use of lights and sirens
The impact of provider fatigue
More and more research has indicated that not every 911 call requires a lights and sirens response, yet there is no sign that departments are changing their policies on a wide scale. More than 20% continue to use lights and sirens on every call, with the fire service being the most likely to do so, and private, non-profit being the least likely.
Fatigue management also continues to be a struggle for many systems, and a source of disagreement between the field and the front office. More than half of field providers disagreed when asked if their organization was taking steps to address provider fatigue. Only 21% of chiefs and 27% of medical directors felt similarly. Sadly, even flight medics and nurses were skeptical, with 33% feeling no steps were being taken, despite the dangers of helicopter EMS.
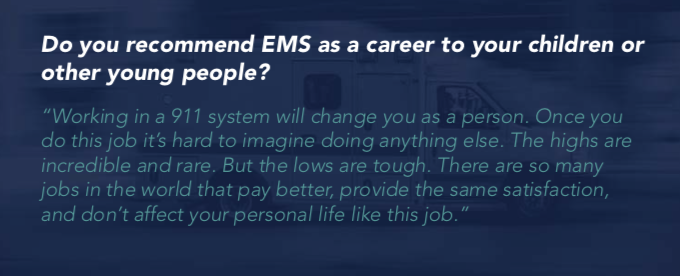
The last few years have seen little shift in the optimism of EMS professionals, with many remaining skeptical that the profession is headed in the right direction. Nearly 40% of respondents said they would not recommend EMS as a career to their children or other young people. This is a significant increase from 2018, when about one-third of respondents said they would not recommend EMS as a career to a young person. Reasons varied, with most providers citing:
Could the next few years mark a turning point, though? Possible changes to reimbursement models, a renewed focus on provider health and wellness, and leaders pushing for increased professionalism all may have a positive impact on the profession. But to truly move EMS forward, we will also need to see better progress on issues that can be addressed by individual providers and leaders at the local level:
Until those basic improvements happen, it’s hard to imagine why the people in the field serving our communities would be any more optimistic about the future of their profession.
Roxanne Shanks, MBA, is a partner at Fitch & Associates. She serves as the CEO for LifeFlight Eagle Air Medical Program in Kansas City, Mo., and also as the executive director for the Association of Critical Care Transport. She has an extensive background in healthcare and EMS leadership with more than 26 years of experience in progressively responsible clinical and leadership roles.
Jay Fitch, PhD, is a founding partner of Fitch & Associates, and is internationally recognized for leadership as a consultant, educator and innovator in EMS and public safety.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...