Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

EDITOR'S NOTE: This article originally appeared on EMS1.com. Special thanks to our guest author, David Wright, MS, PA-C, NREMT-P, for EMS1 BrandFocus.
__
The most important initial care step is to stop the burning process, but it’s also critical to know how to identify the type of burn and estimate the total area affected to help select the most appropriate destination for the patient
You and your partner are responding to a 911 call. Dispatch informs you that your patient suffered a burn. There is no additional information available at this time because the caller is quite panicked.
Your mind starts to race – maybe it’s a child who pulled a hot pot of noodles on top of themselves, maybe it’s a teenager playing with gasoline, maybe it’s a firefighter who was battling a fire, maybe it’s a grandparent who fell on a space heater.
No matter the situation you find when you arrive on scene, there are a few basic principles that apply to all burn patients. Here are 10 things EMS providers need to know to better assess and treat burns.
Every year, approximately 1.1 million Americans suffer burns that are severe enough to seek medical attention. Every 23 minutes a person sustains a burn, and every two hours someone dies from a burn injury.1 These burns often occur in the home, and many of them are classified as preventable.
Most people are at home when they sustain these burn injuries. According to Stanford Children’s Hospital, many of these burns can be avoided with basic household safety precautions.2 While most Americans have a household escape plan (60%), only 25% have reportedly practiced it.
Prevention is the best strategy to avoiding serious burns, as smoke alarms can reduce your chance of burn death by 50%.1 One thing EMS clinicians can do is look for smoke detectors when they respond to calls. Most local fire departments have free smoke detector programs, and this strategy alone can be lifesaving. Other opportunities exist through partnership with the fire department and open houses, where burn prevention and safety precautions can be taught.
When a person experiences a burn injury, the most important initial care step is to stop the burning process. This may seem obvious, but the initial burn cause may transfer to other flammable objects.
Make sure to cool the area to stop skin burns. Clean towels soaked in cool (not cold) water often work well. After approximately 15 minutes, remove the wet towels and replace with clean dry coverings. Also make sure to keep the rest of the patient warm, as you don’t want them to become hypothermic.
Don’t forget to remove clothing that may be smoldering and ensure that the patient is away from the original ignition source.

Correctly identifying the type and severity of the burn will assist you in determining the initial treatment, as well as the ultimate destination for the burn patient.
Burns have two basic classifications: the depth/severity of burn (superficial, partial thickness and full thickness) and the etiology of the burn (thermal or inhalation). Thermal burns are further subdivided into scalds, contact, flame, chemical and electrical burns.3
Inhalation burns or burns that involve the airway are serious concerns for airway compromise. Closely monitor the airway, as the need to secure the airway (frequently via endotracheal tube) is often necessary to avoid loss of airway later in the clinical course.
Partial or full thickness burns covering a large percentage of the body often benefit from skilled management at a burn center, where a burn team comprising medical experts, social workers, therapists and psychosocial experts is available.4
Pain is usually a bad thing when examining patients, but burns can be tricky. It is important to evaluate if the patient is in pain when assessing burn victims.
Sensory nerves that send pain signals to the brain are located under the outside epidermal layer of the skin. When a person suffers minor burns, these are activated, but deeper partial thickness and full thickness burns often destroy the nerve endings, rendering them unable to send pain signals to the brain.
Patients who appear to have a severe burn but are not complaining of a lot of pain are at high risk for complications due to the burn injury.5
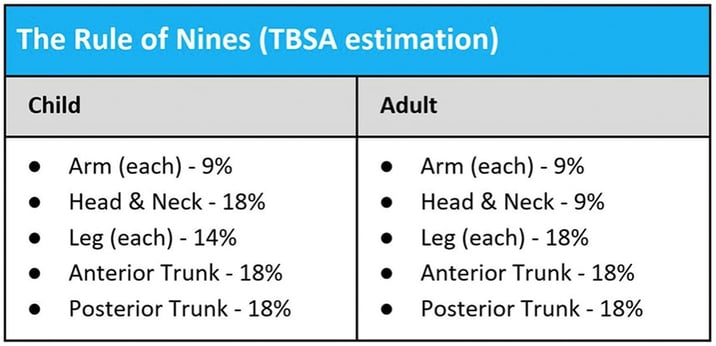
Another key component of burn treatment hinges on your use of the Rule of Nines (see below) to estimate the total body surface area burned (TBSA). Establishing the TBSA affected will often affect the destination (burns greater than 10% TBSA often go to burn centers) and treatment plan.
Don’t forget that only partial thickness and full thickness burns are used to assess the severity of fluid loss.6
The airway consists of the nasal and oral passages and is obviously very important to evaluate – after all, it is first in the ABCs of the initial assessment – and it is no different in the burn patient. Burns to the airway can be subtle and require a thorough evaluation to assure there is no damage to the airway structure.
Unrecognized airway burns can be deadly, leading to a “cannot intubate, cannot ventilate” situation that will likely end up requiring an emergent surgical airway.7 Airway management and evaluation should be performed early and should be continuously monitored for acute changes.
You take trauma to a trauma center and pediatrics to a pediatric center, so why not take burn patients to a burn center? Severe burns, as dictated by local protocols, should be transferred to a burn center. It is important to know your regional centers and the requirements for burn center transport.8
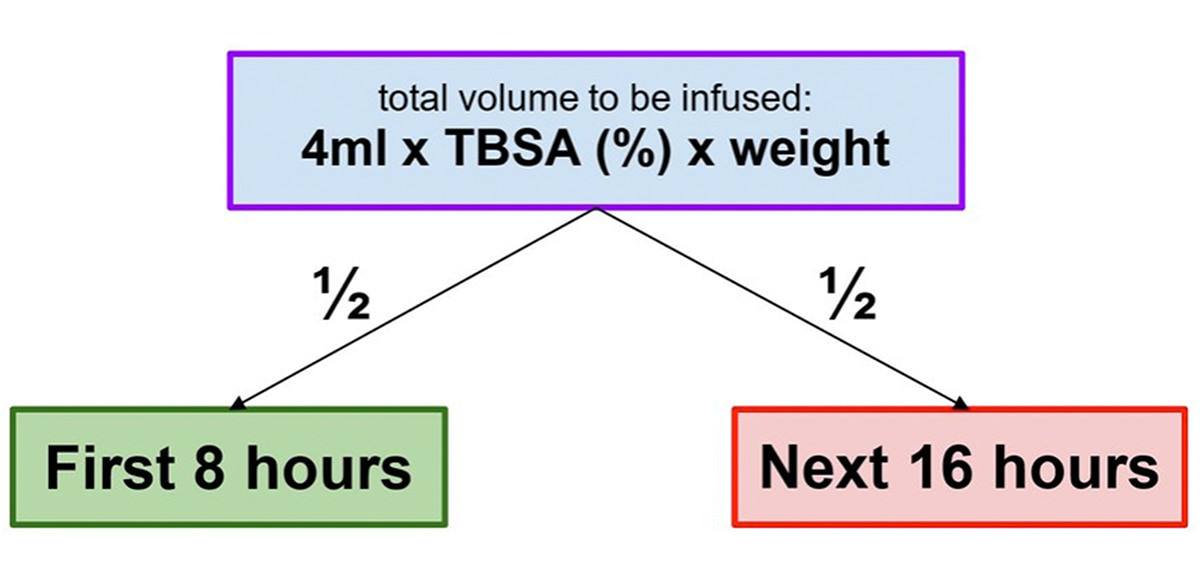
Another problem caused by the disruption in the skin surface is water retention. Dehydration is common in patients with significant partial thickness or deep thickness burns. The use of TBSA and the Parkland Formula (see below) can be a valuable starting place for fluid resuscitation and management. Fluid resuscitation is critical in the initial management of moderately to severely burned patients, especially in those with >20% TBSA, as mortality in these patients is known to be significantly higher.6
To calculate the total amount of fluid to be infused, multiply 4 milliliters times the patient’s body weight in kilograms times the TBSA. This will be the total infusion over the first 24 hours. Half of that infusion goes in over the first eight hours, while the other half is infused over the next 16 hours.
After initially stopping the burning process, you should keep the wound clean and dry.9 During transport, you may want to cover the wound to keep it clean and keep the patient covered. This will preserve heat, prevent hypothermia and assist in infection prevention over time.
Keeping burn wounds clean and dry is essential for infection prevention, as approximately 10,000 Americans die from burn-related infections per year.1
The E in ABCDE is exposure, which is important for evaluation of the burn patient – but after the initial exposure, it is important to cover the patient because the skin is an important component of maintaining temperature regulation, and burn patients can become hypothermic in a very short amount of time.10 Those at the highest risk are those with altered mental status, such as those who receive rapid sequence intubation or have a documented Glasgow coma scale score of <8.11
1. CDC (2020) Burns. Accessed from: https://www.cdc.gov/masstrauma/factsheets/public/burns.pdf
2. Stanford Children’s Hospital (2020). Preventing Burn Injuries. Accessed from: https://www.stanfordchildrens.org/en/topic/default?id=preventing-burn-injuries-90-P01750
3. Johnson, N. J. (2017, March). World Report on Child Injury Prevention. https://www.who.int/violence_injury_prevention/child/injury/world_report/Burns.pdf?ua=1
4. Al-Mousawi, A. M., Mecott-Rivera, G. A., Jeschke, M. G., & Herndon, D. N. (2009). Burn teams and burn centers: the importance of a comprehensive team approach to burn care. Clinics in plastic surgery, 36(4), 547–554. https://doi.org/10.1016/j.cps.2009.05.015
5. Hussain, A. (2018). Surgical treatment of acute burns. Wounds UK, 14(2), 30–37.
6. Moore, R. A. (2020, July 10). Rule of Nines - StatPearls - NCBI Bookshelf. NCBI. https://www.ncbi.nlm.nih.gov/books/NBK513287/
7. Borle, A., & Singh, P. M. (2015). Finding the way into the burnt airway! Journal of anaesthesiology, clinical pharmacology, 31(2), 242–243. https://doi.org/10.4103/0970-9185.155157
8. Wilson Shupp, J. (2018) When to Seek Treatment at a Burn Center. American Burn Association. Accessed from: https://ameriburn.org/when-to-seek-treatment-at-a-burn-center/
9. UpToDate (2020). Overview of the Management of the Severely Burned Patient. Accessed from: https://www.uptodate.com/contents/overview-of-the-management-of-the-severely-burned-patient?search=burn%20treatment&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2
10. Romanovsky A. A. (2014). Skin temperature: its role in thermoregulation. Acta physiologica (Oxford, England), 210(3), 498–507. https://doi.org/10.1111/apha.12231
11. Page, D. & Trembley, A. (2014). Are We Keeping Out Burn Patients Warm Enough? JEMS Vol 9 (39). Accessed from: https://www.jems.com/2014/09/15/are-we-keeping-our-burn-patients-warm-en/
About the Author
David Wright, MS, PA-C, NREMT-P, is a physician assistant at Washington University in St. Louis working in the Division of Pediatric Emergency Medicine. He is a former paramedic who has worked in a busy 911 response service, hospital emergency rooms, and as a flight paramedic. He also currently holds certifications as a Nationally Registered Paramedic, TEMS, EMS Instructor, Clinical Simulation Instructor, Firefighter I & II and Hazmat Operations. His passions include EMS education, clinical simulation and furthering the EMS profession.
![]()
Community paramedics in Teller County, Colorado are pioneering new ways to care for mental health patients using cutting-edge technology. Check out what they've learned.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...