Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Editor's Note: On August 11th, EMS1, Fitch & Associates, and the National EMS Management Association released their fourth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is written by Kris Kaull, B.S., NRP, CCEMT-P, FP-C.
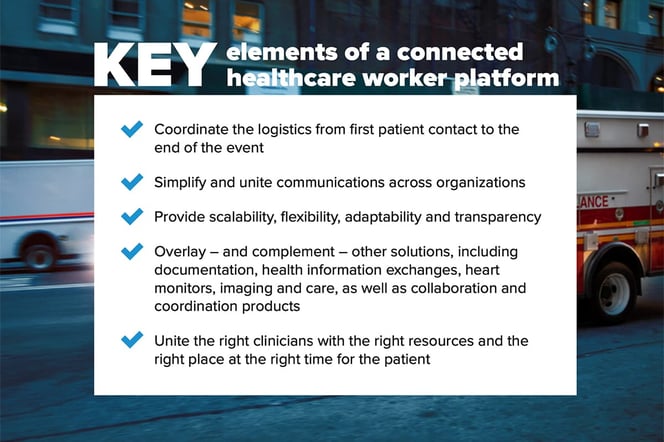
As COVID-19 continues to shape the landscape of healthcare, many profession-altering changes are here to stay. The most impactful of these is the paradigm shift to the “connected worker.”
While this may be a new term in healthcare, it has been covered extensively in manufacturing. As Natan Linder wrote in Forbes, “For years, we interpreted poor manufacturing outcomes to poor human performance (as much as 70% of mistakes in factories occur on human-centric processes). But things changed with the fundamental insight that humans aren’t actually the problem. Badly designed or overly complex work systems are.”
Healthcare faces even greater challenges. There was a time where a healthcare professional may have shined based on their clinical expertise alone. But this is no longer the case. I met with a neurologist in Seattle who told me that she makes, on average, 17 phone calls before she sees a stroke patient. Consider the time-sensitive tasks and coordination that need to be completed by a team in order to properly treat a critical patient: multiple phone calls, pages, answering services, handwritten notes, and radio communications.
Medical errors are a leading cause of death, with miscommunication during transitions of care contributing to 80% of those incidents. It’s a wonder how clinicians overcome obstacles and avoid errors despite archaic systems, siloed organizations and traditional thinking.
As Tom Frieden explained in the Wall Street Journal, the CDC has learned a crucial lesson over the past two decades: “The best emergency responses use everyday systems that are robust enough to scale up in an emergency. Yet efforts to strengthen such systems are often unfocused. Enhancing countries’ capacities will require substantial resources, robust technical assistance and an insistence on accountability.”

This should come as no surprise. Consider the traditional multiple-patient incident training. These semiannual (if that) exercises are both a disservice and a dangerous practice that contribute to a false sense of security. We know that, almost without fail, communication logistics and systems fail during an incident. Why? Because when there is a stressful event, humans revert to what they know and the tools they use regularly.
Instead of the yearly tabletop drill or all-hands training, training for high-stress events should be incorporated using the same systems used for the routine responses during monthly continuing medical education hours. More importantly, clinicians need access to everyday systems that can scale in an emergency.
Download the full 2021 EMS Trend Report here
What happens when a high-stress event such as a multiple-car crash, active shooter, tornado, ice storm, wildland fire—or even a worldwide pandemic—occurs in your region? Although the major challenges will differ according to your area’s size and resources, the need to standardize and simplify logistics, communications, and data is imperative across the board.
EMS and hospital staff can instantly and seamlessly communicate event-based patient information, including one-tap team notifications, image sharing, audio/video calls, ETA alerts, and more from the Pulsara app. Public safety, emergency management, and public health can be easily involved when needed. Transparency keeps everyone informed and minimizes miscommunication.
Imagine the start of a 24-hour shift. The morning consists of truck checks and a few 911 requests. Midday, they respond to a female having chest pain. EMS alerts the receiving hospital using Pulsara, effectively replacing the radio report. With the heart monitor integrated, the ECG is seamlessly transmitted, along with vital patient monitoring information.
The emergency department receives the alert and activates the entire STEMI team, the patient is registered prior to arrival, and paramedics can bypass the emergency department directly to the cath lab – all on a patient-centric communications and logistics channel.
As the crew completes their documentation and grabs lunch, they are requested to emergently transfer a trauma patient from an outlying rural community access hospital to a receiving Level I trauma center. Prior to their arrival, the attending doctor connects to the trauma specialist through live video consult via Pulsara. The patient is accepted, and both logistics and communications are streamlined, saving both the patient and care team critical hours.

Later that day, the ambulance crew arrives at the home of a patient who is sick but not critical. Through Pulsara, they alert their mobile integrated healthcare team. The community paramedic arrives on scene, communicates via live video with their online medical director, connects the patient with their primary physician, and helps them create a healthcare plan. The ambulance crew remains available for time-sensitive emergencies while the patient is more appropriately treated with the right services.
Over the course of that shift, the use of Pulsara united disparate teams across organizations. By using a standardized tool, the care teams created the building blocks for daily healthcare communication hygiene and are positioned to easily scale their care systems if a more severe emergency occurs.
Most importantly, this new reality allows clinicians to focus on what they do best: patient care.
About the Author
After beginning his career as a firefighter and EMT, Kris Kaull started paramedic.com and then co-founded EMS1.com, which today is a leading online paramedic resource. He's worked as a firefighter captain, paramedic and ambulance service director and, most recently, practiced as a critical care flight paramedic covering rural Montana and Yellowstone National Park. He is currently the Chief Marketing Officer at Pulsara, a healthcare communications technology company. As Pulsara’s CMO, Kris leads the company’s efforts in expanding market reach, partnership development, and overall strategic business growth.
Pulsara is helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...