Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

What if you could improve patient care—across your city, region, and even state—by streamlining communication and coordination between EMS and hospital teams? Texas hospital and EMS leaders are doing just that, utilizing new workflows built on a scalable telehealth communication and logistics platform. Since reworking their trauma system, they’ve improved efficiency, reduced phone calls to multiple people, streamlined transfers, optimized continuity of care, and created shared awareness and accountability.
In this leadership roundtable with Jennifer Carr, MSN, RN, CPEN, TCRN, Vice President of Trauma Services at CHRISTUS Spohn Health System in Corpus Christi, TX, Randy Endsley, BSN, CFRN, CEN, LP, CMTE, Chief Medical Officer and Flight Nurse with HALO-Flight in Corpus Christi, TX, and Corey Ricketson, Sales VP at Pulsara, discover why they created this new system of care, what day-to-day operations look like, and how they are growing it across their organization and region.
Watch the full webinar and check out part 2 of our blog coverage below! And in case you missed it, catch up on part 1 here.
NOTE: This transcript has been edited for brevity and clarity.
Corey Ricketson
One of the things we’ve realized is that it's obviously great if somebody comes straight to your trauma center. But, it turns out that people will go to the nearest facility—and maybe it’s somewhere that can't take care of them. Or, for stabilization purposes, EMS says, “We’ve got to have an airway. We've got to go to the first facility first instead of to the trauma center.”
All of those situations happen. Talk to me a little bit about how this improves moving from one facility to another facility, and how we inserted Pulsara into that mix.
Jennifer Carr
So if EMS utilized Pulsara for the patient that they took to one of our level four trauma centers, the ER would receive that. If they identified that the patient had injuries that needed to be transferred to a higher level of care, we then would use our Christus Command Center, our transfer center, and bring them in the loop on this, and they would be added into the Pulsara channel. And then we would reach out to the level two trauma center and communicate to them that there's a patient that needs to be transferred to them. The trauma surgeon on call and the ER physician would receive the information on it. And then when EMS picks the patient up—whether it's air or ground—from the level four facility, they could be added to the channel, too.
And so whenever they were transferring the patient to a level two trauma center, and they were sending in their report, the receiving hospital could see all of this information, from the time of the mechanism of injury through the ER at the level four facility, through the transport—any changes in status, any pictures. And so it was really good information. It wasn't a lot, but it was the key information that needed to be seen and communicated to help ensure we had exceptional patient care.
Randy, do you have anything you want to add on that?
Randy Endsley
So I haven't experienced from the facility [side] yet, but what I have experienced is from the EMS crews themselves. I think I touched a little bit on that. It's kind of just that same continuity of care. I don't know if you know how air crews are, but we have a very small amount of time we're supposed to spend in the back of that ambulance. It is quick, quick, down and dirty, and there are going to be things you forget to ask. Pulsara allows the chance for them to put that information in there before all that happens—and even add it after we've left, that's the great part. I'm looking forward to seeing the other side of this as we go forward. And like Corey said, we're a year into this and look how much we've done already. So in the coming year, I'm sure that we'll see a lot more of this.
Corey Ricketson
If we look at the “crawl, walk, run” phases, I think it would be safe to say we're sort of in a slow jog right now. We have added the transfer center into the mix. So just to be clear, if EMS started a channel and took it to a primary hospital, that channel already exists. And now the primary center just simply adds the transfer center into the channel with them. And that alleviates the first 15 questions on a phone call, which are: “Where are you calling me from? What is your name? What is the patient's name? Could you please repeat that? What's the injury that this patient has?” All that information is in Pulsara already, so it speeds that process up.
I think as we get into the “run” phase, what we're going to see—and I'll talk about a couple of ways that this can happen—but that sending facility then adds in the transport resource into the same channel. That way, you know, we've got some really high-powered resources on the other end at these trauma centers that are waiting to receive that patient, and they're not sure if they're going to get here in 15 minutes or one and a half hours. It's sort of this dead zone or this black hole. And so by adding those transport resources into that channel, they can say, “Hey, we're with the patient.” And Randy can say, “You know what, they're decompensating. We're going to take a moment, go ahead and intubate.” So now, when they get there, they're actually going to be intubated. That was information we didn't have before. And these things change on a dime a lot of times with these critical trauma patients.
So, Randy, getting into that, this is a recent case that you were on. We've got some screenshots, so maybe it looks familiar, but this was a 73-year-old patient that had a tire blow up in their face. You were on this flight. And it's not the most critical of trauma patients, but I think it does a good job of illustrating what happens with that continuous communication and that handoff process. So walk us through a little bit of what this particular case was.
Randy Endsley
So the interesting thing about this is, this was maybe the third or fourth time that EMS had started to bring us into the channel first. We had put out instructions through the Coastal Bend Regional Advisory Council (CBRAC) on how to do that. And we're starting to see more and more of this. In fact, I had one last night myself, where they included us in the channel right away.
On this call, the radios in their truck were not working. So without Pulsara, we would have had almost no information going in. And, you know, air crews, we're spoiled. We like to know what we're going into. We need to know what bags we need to take in—do we need to take our blood in, do we need to—all these things. I was able to basically chat back and forth with the medic on scene, asking him all these questions. He was giving the report, and I was asking him questions back and forth. So this was a great example. My partner and I even stated that afterwards during the flight back, saying, “Wow, look what Pulsara did for us on this flight.” We would have gone into this not knowing anything that was going on, but we were able to actually communicate back and forth, even from 2,000 feet up in the air. It worked really well.
Corey Ricketson
So you've got this ground crew that basically puts in a quick Pulsara report and puts in some information. They probably took some pictures (which I can't show because of HIPAA) as well. But then they basically add you into the channel as you launch because they know what ship is coming to their location. And so we can see here that they've put in some of that information.
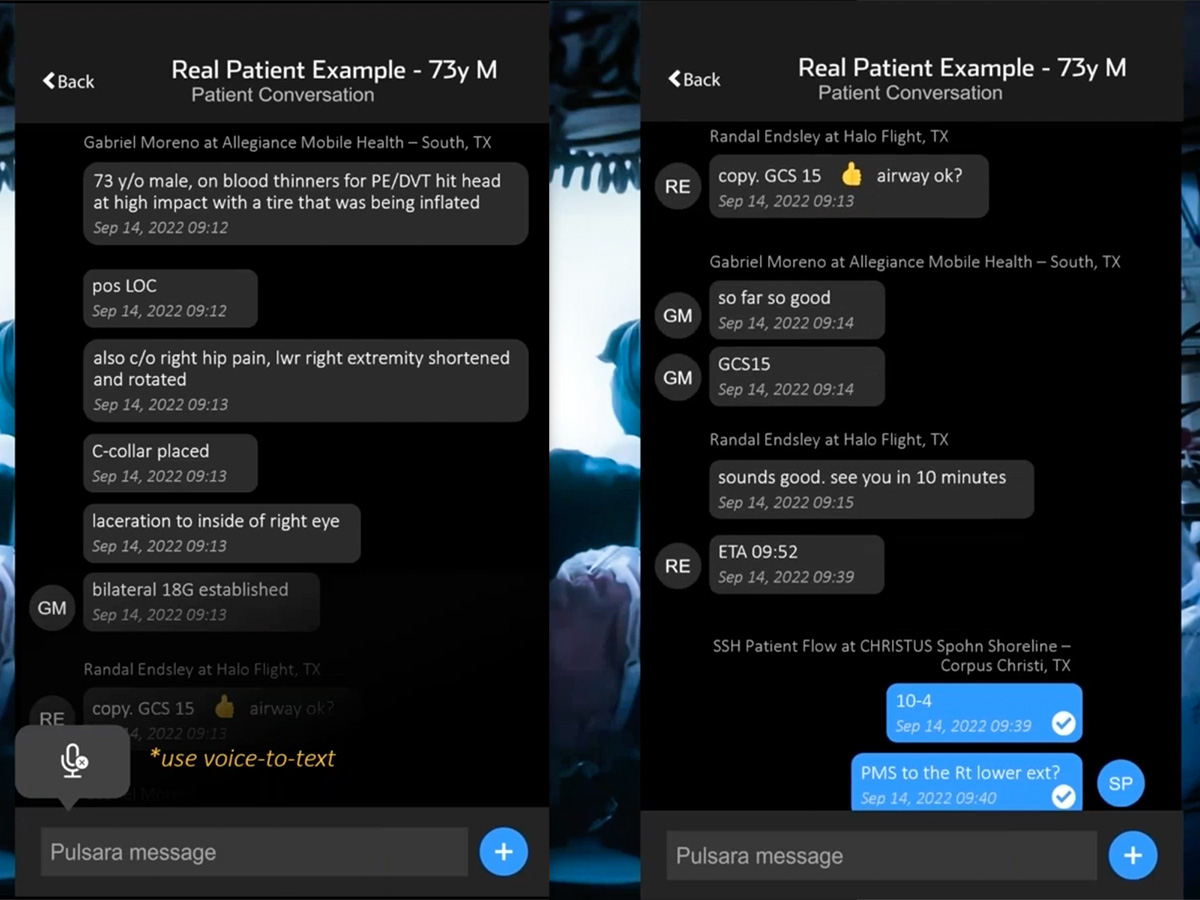
And then as we scroll through here, Randy's actually talking to them, going, “Hey, how's our airway look? Is there anything I need to grab out of my bag to deal with an airway?” They're saying, “No, GCS is 15, airway looks good.” You're still 10 minutes out, and you're telling them what your ETA is while you're in flight. So that's excellent.
And then in the next part of this, you're actually sending the report to the hospital, and there's a patient flow coordinator at Shoreline that’s kind of a paramedic position. They take a lot of the initial communications and they may assign room numbers, or get patients in the particular trauma categories that need to be in—so they're even asking you questions while you're in flight as well.
Randy Endsley
I was able to add more to the chief complaint [section] and added some things that I wanted the trauma center to know. Having worked in ERs before, I know exactly what it takes to get a level one activation versus a level two activation, so I know the lingo and the vital signs that they're looking for. I want to make sure that they had all the information [they needed] to make a good choice.
Corey Ricketson
Awesome. We mentioned that there is a way to add the flight crew in immediately, even before they've gotten to their location. But we also are spoiled in Texas. I want to talk very quickly about wristbands. We have a statewide wristband. I would really encourage any state, whether you're using Pulsara or not, [to consider it]. A statewide wristband has huge implications and merit from a continuity of care and a patient tracking standpoint.
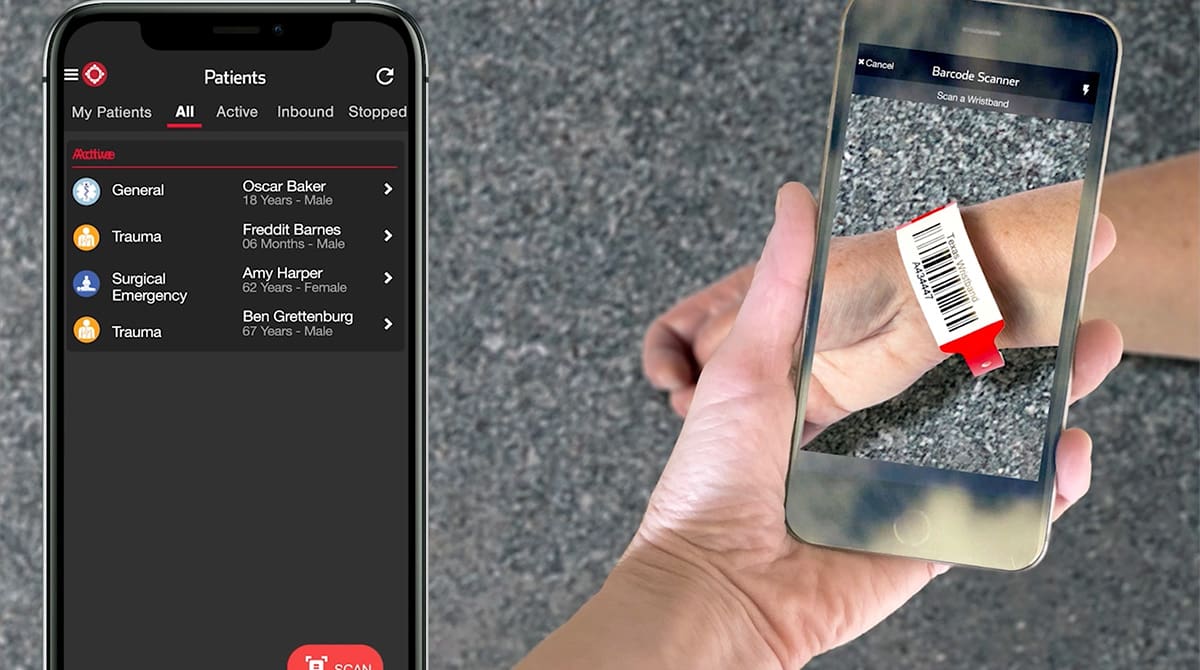
We actually baked technology in Pulsara where we can scan that wristband. EMS simply puts a wristband on a patient. A patient can be banded on initial patient contact, wherever that takes place, whether that's the tertiary or the primary care facility, or whether that's in the field by a first responder.
Once that band gets put on a patient, we scan that band in Pulsara. And if that ground crew had scanned the band and [created a patient channel], and Randy had flown in and now goes to that patient’s side, it’s as simple as scanning the wristband in Pulsara to be added into the channel. So along the way, anybody that comes in contact with that patient and has a responsibility for the care of that patient can scan that band, no matter what organization they're from. They're added in, and they can collaborate and communicate with all of the folks that are in that channel.
We had an interesting situation in Corpus, actually, where even the freestanding emergency departments use Pulsara. They put a band on a patient because they needed to transfer them out (it was not a trauma patient). They scanned the band, and the sending hospital took a picture of a chest x-ray, took a picture of lab values, and put in a working diagnosis. That patient ended up leaving in a privately-owned vehicle, against medical advice, and showed up at a different location. That hospital was able to scan that band, and they were added into that same channel with the sending hospital.
So pretty cool stuff. This is kind of our hurricane evacuation plan too, which we'll get into in just a second.
I know that we're not completely in that run phase yet, as we're a year into this. But Randy or Jennifer, since implementing this, what are some of the biggest benefits that you've seen? And has there been anything that you really didn't even think would be a benefit?
Jennifer Carr
I mean, really, it's communication: good communication with all of the team that's caring for the patient. When the trauma team is responding to the patient, it's very helpful that they know more about the patient, know the vital signs, and know the injuries, and are already starting to think of their plan of care for that. And so that's probably the win is improved communication, which in turn makes improved patient care.
Unforeseen benefits from a trauma program perspective are: our ability to turn around and use the reports and audit tools in Pulsara for accountability. We can go in and look and see exact times of the activation, the times for EMS, the times that it was activated, and that the trauma surgeon received it. And so for us, from a performance improvement perspective of a trauma program, to be able to [use] all the behind the scenes tools to help us with important performance improvement of a trauma program. Also, sometimes it's hard for a trauma program as we don't know who the ground EMS was that called the flight service, and we know the fire service that brought the patient to them, but we don't know who that ground service was. And so we can use Pulsara to look in the report and see, “Okay, this was Allegiance EMS that was the first on scene. And then they brought in Halo Flight to transport the patient to the hospital.” Getting more information that we need for our trauma programs—our trauma registry—has been a valuable and unforeseen benefit.

Corey Ricketson
Randy, I’m gonna pick on you again. Actually, this was a really good move on your part. You were one of the first to adopt this in the Coastal Bend, even though you didn't have a hospital in the Coastal Bend to actually take a patient to yet, because we had just pulled the trigger and everybody decided this is the way that we're going to move.
But as you mentioned, you guys have ships and transport far beyond the Coastal Bend RAC. So tell me a little bit about how you're able to utilize this not just in your little home area, but in other areas that you serve.
Randy Endsley
Yeah. So when I heard about Pulsara, this was my answer to going to other cities because we don't always transport into Corpus Christi, because our service area is so big. Sometimes we end up in San Antonio, sometimes we end up in Laredo, sometimes we end up in Rio Grande Valley.
And so San Antonio for me was a real problem. Satellite phones are 50/50. They’re hit-and-miss. Sometimes you get them, sometimes you don't. Sometimes they can't hear you. They’ll say, “Sounds like you're in a helicopter. I can't hear you.” and I’m like, “Yes, I'm in a helicopter.” If CBRAC had never gone with it here in this region, I would still be using Pulsara. Because if nothing else, it helped me in those other areas where we were transporting to where they had no radio communication with them, and I had to rely on satellite phone, which I'm just not a fan of, from experience.
So for me, communication, and going into all those other areas. We were number one to try this out, and I wanted to be that—I’ll brag on Halo Flight—we always like to be the trendsetter, and so we were glad to take that on. We're a small organization, so it was really easy to implement, and we hoped that people would follow.
Corey Ricketson
I would say that your flight services typically have a lot of respect from your ground services and the hospitals and others in the healthcare continuum. And so for you guys to get on quickly really showed a positive example to others that, look, we think this is a good thing. We are endorsing this. We're leaning in, and we're going full speed ahead. So I think for those ground crews, they looked at that and said, hey, Halo Flight’s doing it, we should definitely get on board. And so that was just a really good example too.
Randy Endsley
I make sure to tout all of our experiences and successes with Pulsara while they were thinking about, “Hey, do we want to do this?” I’m like, “Hey, let me tell you about this story, and this story, and how it improved patient care.” And so, yeah, it was a good thing.
Corey Ricketson
So with that said, you know, we've talked about how Pulsara isn't just a stroke, trauma, or STEMI solution. This is a system of care solution in general. And unfortunately, we have things like hurricanes. We have mass shootings. We have migrant populations coming through the border that then jump out of an 18-wheeler 100 miles in because it's 120 degrees in the back of that 18-wheeler. So we have these mass casualty events. Jennifer, talk to me a little bit about what your vision is for Pulsara in some of those large events as well.
Jennifer Carr
So for large events, we have trained within our whole Christus Spohn system to use the Texas EMS wristbands, the teal wristbands, that they will be on all patients, and that there will be designated people within all of our facilities that are able to go around and scan these patients’ wristbands. And you can even take their picture if you need, or take a picture of their valuables.
And in the event of an MCI, in the event of an evacuation such as a hurricane, or any type of disaster here in Corpus Christi, we definitely have a lot of risk. We have the refineries. We have the port to worry about, as well as hurricanes.
But we have a way that we can track our patients. And this is something that we learned from Hurricane Harvey. We evacuated our patients out of the system—north, or to safer areas—but it was hard to keep track of where they went. And especially if somebody reached out to us and said, “Where is my family member?” [it was difficult] to communicate exactly, “They are in room 403B at University Hospital in San Antonio.”
With this method, we can use Pulsara to track our patients, to transfer our patients, and to keep track of them for communication and continuity of care.

Corey Ricketson
Yeah, I think the important building block there is that because these people use it every single day, it becomes a ubiquitous part of their life. And so when they think emergency communications, it's Pulsara. And no matter whether it's the toe pain that's going to go to triage, or it's the mass shooting where we've got 30 patients and we're distributing that load, we're actually doing the exact same thing, and we've made that really natural for ourselves so that this feels natural in our hand and it's what we're using.
We did kind of expand the solution recently and have participated in some large-scale events. And this solution does have a mass casualty or an incident command type structure to it as well that can scale up and allow an incident commander and others that are managing these events to see at a macro level how many patients are being tied to this particular incident, and where they're going, so that at any given time they've got kind of their finger on that pulse, if you will.
We're in that jog phase. Jennifer, what does the run phase look like? What do you see as some other opportunities to expand this? Not in trauma, but maybe in other parts of the system?
Jennifer Carr
Outside of trauma, we definitely want to get this hardwired for all patients that are being transferred, maybe to a higher level of care, or patients that come in via EMS and we need to activate a STEMI, a stroke, or a sepsis. And even for mental health—we know that there is a crisis with mental health. How can we take care of this population and better communicate?
Corey Ricketson
Yeah, your police department had reached out to us recently to say, “Man, could we have Pulsara, so that when we have one of these mental health or substance abuse patients, we could contact mental health facilities through this and help alternatively navigate those folks?” Because so many of those patients end up in the ER and are there for 24 or 48 hours and are sitting on your wall because they can't get in somewhere. So it's a great point.
As we wrap up, what's the tidbit of advice that you could tell another region or health system, “Here's how to do this right and get the most out of this.” How should you implement this thing the right way?
Jennifer Carr
Take your baby steps. Don't wait to have the perfect process in place. Know that you're just going to start small. You're going to have opportunities for improvement that you identify, but just keep moving forward. Don't wait to have this whole process figured out from start to finish. Just take it in steps, and as you figure out this step, you're kind of working towards the next step. When we broke it down into pieces like this, this made it easier to get going faster. It just made it an easier project to deal with.
Also: communicate with your IT department, your HR department, and your administration. Communicate the wins up front, especially when you talk about patient safety, communication, and continuity of care. And then, of course, the HIPAA compliance of this. There were some security concerns because, you know, this is on iPhones and iPads. And so assuring them then that you can run audit trails, and that this really is a secure [platform]. Giving that information up front will help to get buy-in from your other departments that are needed for this.
Corey Ricketson
Awesome. So we have a couple of questions from the audience.
Q: Does Pulsara integrate with ePCR software?
Corey Ricketson: Absolutely. We have a public API. We are completely agnostic, and we will give our data to whoever needs to consume it. So with that public API, we have several ePCR systems already that have consumed that and have working interfaces, and then a couple of others that are actually in the coding process right now.
We always hear from EMS: “We don't want to double document.” And I can tell you after teaching this, there's not a lot of manual data entry with this system. It's scan wristband, scan driver's license, take pictures of things like vital signs on your cardiac monitor screen, and then you're not having to manually type this stuff in. Talk-to-text on a chief complaint really mimics a radio report. So there's nothing manually that I'm having to document. But yes, it would be nice if, at the end of that, I could press an import button, and now those demographics and my at-patient time and certain things like that flow into that ePCR.
Q: Does it replace the radio report?
Corey Ricketson: Initially, we did a little dual process, but that quickly ended. We don't want people having to do double the work. So this gives a lot of information quickly and things that you can't give over a radio, like a patient's name, or a picture of injuries, or 12-lead. So we're really sending a bolus of information with a lot better info for the ER to make decisions off of. And there's no need then to send a radio report. And in fact, as soon as the hospital actually clicks into a channel and sees the report, it automatically sends a message back to EMS saying that the hospital acknowledges, and now there's a handshake so that they know it's been received on the other end.

Q: Can you access patient information later, and how long is this stored?
Corey Ricketson: We are hosted through the Amazon Cloud, and in the United States, that information is not purged. Of course, we have different rules across the pond that we live underneath, as well. But for the United States, we don't purge the data. If I'm an administrator, I can go in retrospectively and run some of that data that Jennifer was talking about. And I'm sure Randy looks at these cases after they've been completed for QA/QI purposes. It's one of the requirements to be able to do that 100% review. So seeing all of that information and being able to retrospectively look at it and dissect who did what, when, and if there's been any delays or hiccups, they can put their finger on that.
Jennifer, one more question for you and Randy: what are some of the challenges that you ran into? One of the things that you might touch on here is that trauma surgeon on-call thing.
Jennifer Carr
Oh, yes. So one of the things with Pulsara is, you're logged into the app, but you log yourself on and off call. And so we noticed that, and we got our trauma surgeon set up, but when we would go back for our auditing and look, they didn’t receive the activation. And I was like, “Well, they're on call.” Well, they forgot to log themselves on call. And so we’d remind them, “Hey, you're on call. Remember to log yourself on and remember to log yourself off,” because they definitely don't want to receive an activation when they're asleep and they should be off call. And so we worked with Pulsara, and where we upload the trauma surgeon call schedule monthly, we do a month at a time, and they do 12-hour shifts.
And so we uploaded it into a calendar, and it automatically logs them off and on call. It's been amazing. That's probably been one of the huge wins of this. It automatically logs them off and on call, so we don't have to worry about that. They have been very pleased with that process change.
Randy Endsley
For us, the change to Pulsara, believe it or not, has been really seamless. It has not had many challenges for us. It’s really just learning the system and utilizing it. There are some times still where our hands are too busy to get on our phones, and sometimes we do end up using the radio. I would say the same thing as Jennifer, though; my crew has to remember to log themselves in every morning. But we just make it part of our our preflight duties.
Corey Ricketson
Yeah. Like last night, you had a five-minute flight, so you’re up and down, and there are a lot of operational things that we worry about for safety reasons in the air. It's not just patient care. But the cool thing is that the ground unit started that channel. They can actually send right to that hospital on your behalf and say, look, Halo Flight may call you, but here's what they've got, because we're the ones that originally started care. And if you're in flight, and they find patient medications or want to take other pictures of things like mechanism, they can just keep adding that stuff to the channel, so that when you land, the hospital has it, you have it, and that continuity of care is not lost.
I know we're down to one minute here, but I have one more question I wanted to address, and that's on regional competition. One of the things I can say that I've been really proud of in Texas is that we are broken down into these RACs. And each of these RACs has multiple health systems that are in competition with each other every single day.
But what I find is that these RACs breed cohesion in a lot of ways. And so even though we know that we're competitors, we're still moving forward at a macro level as a region for the betterment of that patient. And so you still have your proprietary processes. We're not giving away any of that. But because we've standardized a way to communicate, everybody benefits.
Because at some point, the MCI is going to happen where we all have to share the load. At some point, we're going to need to evacuate that hospital because the hurricane comes in. At some point, X, Y, or Z happens, and we have to be on the same page and collaborate. And if we're siloed, that breaks down. And COVID really brought that to light, and that's the reason that we got the state contract in Texas, so that we could standardize how we move patients and how we talk to each other across the state.
What does it take to build a system of care that scales? Eric Epley, Executive Director of the Southwest Texas Regional Advisory Council (STRAC), and Corey Ricketson, Pulsara's Sales VP - Texas, discuss the benefits of using the same communication platform for everyday patient transports, transfers, and transitions of care and stress events. Watch the webinar here!

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...