Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
What if you could improve patient care—across your city, region, and even state—by streamlining communication and coordination between EMS and hospital teams? Texas hospital and EMS leaders are doing just that, utilizing new workflows built on a scalable telehealth communication and logistics platform. Since reworking their trauma system, they’ve improved efficiency, cut down on phone calls to multiple people, streamlined transfers, optimized continuity of care, and created shared awareness and accountability.
In this leadership roundtable with Jennifer Carr, MSN, RN, CPEN, TCRN, Vice President of Trauma Services at CHRISTUS Spohn Health System in Corpus Christi, TX, Randy Endsley, BSN, CFRN, CEN, LP, CMTE, Chief Medical Officer and Flight Nurse with HALO-Flight in Corpus Christi, TX, and Corey Ricketson, Sales VP at Pulsara, discover why they created this new system of care, what day-to-day operations look like, and how they are growing it across their organization and region.
Watch the full webinar and check out part 1 of our blog coverage below!
NOTE: This transcript has been edited for brevity and clarity.
Corey Ricketson
Welcome, everyone. Thank you for joining. I hope that you find this presentation very informative and something that you can use back home. I know everybody's doing a lot of really good work, and things are extremely busy, so I'm really excited today to highlight one region and system in particular that I'm pretty proud of. Today we're going to be joined by Jennifer Carr, VP of Trauma Services for the Christus Spohn region, which is in Corpus Christi.
We’re also joined by Randy Endsley from Halo Flight, Chief Medical Officer and Flight Nurse.
And then I’m Corey Ricketson, [Sales VP - Texas] at Pulsara. I've been here almost four years now. My upbringing in health care was as a paramedic for Austin Travis County EMS, both on the ground and the air side. I was also on our statewide disaster committee.
Jennifer Carr, VP of Trauma Services, will now introduce herself and give a little bit of her background.
Jennifer Carr
I have been a registered nurse for 20 years. I was an emergency pediatric trauma nurse leader and I currently now work for Christus in Corpus Christi, Texas, as a Vice President of our Trauma Services. We have one level II trauma center and four level IV trauma centers. Also, I'm very involved at the state level with the regional advisory councils, with Stop the Bleed, with Texas Trauma Coordinators Forum, and the Society of Trauma Nurses.
Randy Endsley
Good afternoon, I’m Randy Endsley, and I have 26 years of nursing experience, all the way from ER to ICU, neurosurgical ICU, and trauma center. It’s my 24th year flying as the chief flight nurse and chief medical officer. About 75% of my duties are administrative, but I do fly once a week just to keep my foot out there and keep my skills up. HALO Flight is a nonprofit organization, one of the few left in Texas—only one of two. We have six helicopters, three bases, and we love serving in our Coastal Bend area in Texas.
Corey Ricketson
Awesome. Thank you, Randy. So just so that everybody has a little bit of a lay of the land—in Texas specifically, we have regions. They largely follow the same geographic area as our hospital preparedness regions. We call them RACs. They're just regional advisory councils. And their primary purpose was to really streamline trauma care within a region. However, they do have a vast responsibility and oversight from all systems of care. Things like PPE and any number of different initiatives fall underneath the RAC.
The Coastal Bend RAC specifically is down in southeast Texas. You can see they cover a large swath of the Gulf of Mexico shoreline as well. And in here you do have some urban areas like Corpus Christi proper, but there is a lot of rural area in southeast Texas with a lot of farmland and ranch land and things like that.
So we're going to talk a little bit today about how this region came together and tried to tackle a number of different initiatives. But we're going to specifically talk about how they tackled trauma systems of care within that region.
Jennifer, in looking at this, I'm sure that your problems are not unique to you. I think the audience would appreciate knowing at a macro level, what are some of the big issues that as a region you guys decided you wanted to tackle, and why?
Jennifer Carr
As a region, we really needed to ensure when we had patients that were coming to any of the emergency departments that there was continuity of care. That information was communicated clearly to the team from the prehospital. And if the patient was then transferred to a tertiary center, that information was communicated clearly and nothing fell through the cracks. We just wanted to make sure that we reduced any issues in communication and got our patients through the system faster.
Corey Ricketson
In the next slides we are going to talk extensively about workflow and how we've been able to problem-solve here, so I want the audience to just understand a little bit about what Pulsara is, if you don't have any idea. And really, why we exist is probably the most important thing.
This particular diagram shows a patient moving through a typical system of care, and it doesn't matter if that's a trauma patient, a STEMI patient, or a stroke patient.
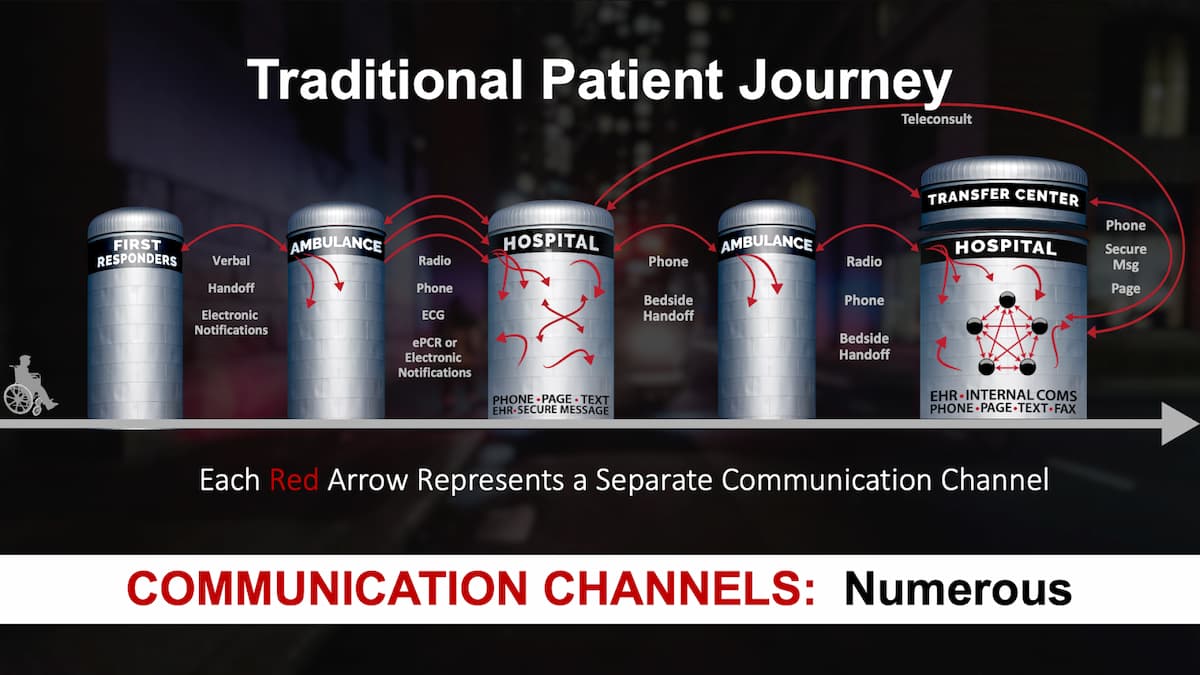
If we start all the way to the left here where maybe a first responder gets notified via 911 and they show up to start taking care of a patient, they're jotting down vital signs and doing assessment information. Maybe they take an ECG. And then when the ambulance shows up, they give a verbal handoff. I call it the “what you got” syndrome. The ambulance gets there and says, “What you got?” And so the first responder gives them a verbal handoff of that information. And it's incumbent upon somebody like Randy to try to remember that information and digest it at the same time that they're assessing [the patient for] themselves and formulating a treatment plan.
And then if they call over a radio to a hospital, there's somebody on the other end of that [at the] hospital that’s listening to that radio report and trying to jot things down. And we all know how that goes sometimes when it's chaotic. Did I miss something? Did I misinterpret something and write down the wrong thing? And then if that hospital says, “well, this patient's a little bit critical, we need more team members,” some semblance of this process is probably what you go through where you call a PBX operator. You say, “I've got this patient that's critical.” They start looking at call lists, sending out pages or phone calls that are one-way communication. If the patient needs to move to a tertiary care center, that's probably a phone call to a transfer center, where you're, again, telling the story, and somebody on the other end is jotting that information down, and then they're calling specialists in order to get acceptance for the transfer and then brokering transport from one facility to another.
And it probably turns out that the ambulance or helicopter that's taking them to the second hospital is not the same one that took them to the first hospital. So we see a lot of opportunity not only for red tape that causes slowdowns in the movement of that patient, but also critical communications loss and breakdowns as well.
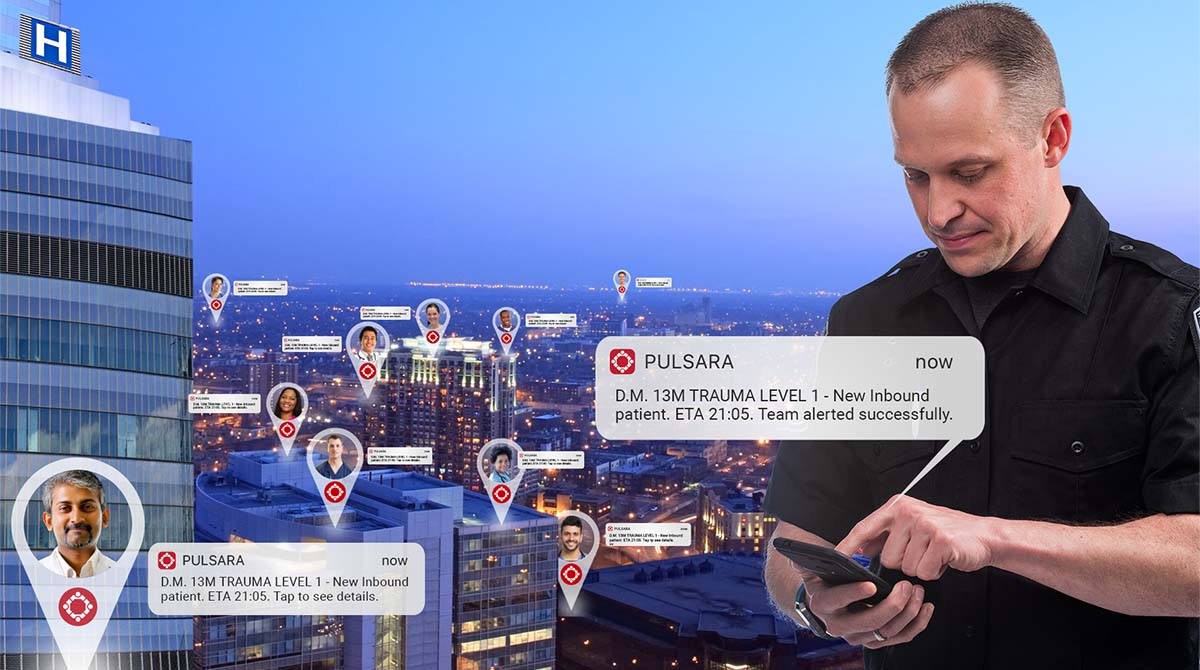
Pulsara essentially creates a communications channel for a dedicated patient. Think of it kind of like a group chat. If we were going to coordinate a dinner tonight with five of our friends, we would probably start a group chat. And then if Jennifer wanted to add someone to that group chat, she would just add somebody. And if I was going to be late to the dinner, I may say, “Jennifer, could you just post a picture real quick of the menu so that I could look at that and tell you what I want to order?”

Pulsara is no different. We allow a patient channel to be created for a specific patient event, and it's all secure and encrypted. Normally, we step into a healthcare environment, and we're back to faxes, phones, radios, and antiquated technology because of HIPAA. With Pulsara, it's completely encrypted and secure, and we can communicate in ways that we normally communicate in everyday life, like group chat. We can upload images and even do live video that can be recorded so that we can put eyes on patients. The key is that we put everyone into a unified patient channel, and that patient channel can expand as the patient moves through the system. Maybe that first responder starts the patient channel and puts in a little bit of information. Maybe some demographic information, maybe they take a picture of an injury.
When that ambulance arrives, they simply add them to the same channel, and then they could start to build teams if they need to. Let's say I need a medical director to remote in with me and look at the patient for some orders. That’s completely feasible within Pulsara. But instead of calling over a radio to that hospital, they send the alert through Pulsara, which allows the hospital to take immediate action and add other team members if needed—a trauma surgeon, x-ray, things like that. Instead of that phone call going to a transfer center, it could actually be pulled in directly through Pulsara, so that they have all of the information that they need in order to start that transfer process.
And then let's just say it's HALO Flight that gets added into the channel for that transport. The great thing is, we are all in that channel, and if Randy comes in later in the game, he can catch up on everything that happened from the initial patient contact with that first responder.
Just to give you a quick example of creating a patient channel, this is going to be a simple trauma case. I just want to show you what the user interface looks like before we go through the next slides. I'm just starting a new case. We do have things like driver's license scanning. We can scan a lot of different things within Pulsara. That dumps the demographics of that patient already into that channel.
I can take pictures of injuries. This does not store to my camera roll. It's all HIPAA compliant, so it's in the cloud. I'm choosing a trauma patient here that we're going to be treating, and then I may even do talk-to-text in order to give a chief complaint. This is not dissimilar to a radio report today. It just puts this into text now so that anybody on the other end can read that and consume that information quickly. And then I simply select a destination. It does auto-calculate ETAs and things like that.
Okay. So now that we have a little bit better understanding of what Pulsara is, Randy, I've been a flight medic as well, and so I share in some of the frustrations. It'd be nice for the audience to know if they've never been on an air ambulance crew, what some of the challenges are when we fly in and we're going to be taking over patient care from somebody. What are some of the things that we run into out there?
Randy Endsley
Well, number one is, communication is always the issue. Sometimes the channels that you use to communicate with your EMS are great, sometimes they're not. There's the old joke about gremlins. It worked fine yesterday, why not today? Or, there's just mechanical failure. So sometimes you don't get all the information that you would like to get.
[With Pulsara], it's been nice to be able to start getting that information. Even as we're taking off, we're already getting alerts from EMS, and they're showing us pictures of the car or pictures of the scene. So the frustration is almost always communication, and Pulsara has definitely helped get around some of that.

Corey Ricketson
Yeah. I remember landing and maybe grabbing a patient quickly. And then, as soon as I'm in flight, I'm thinking to myself, “Wow, I wish I would have asked this question.” Or, “How much Vecuronium did they give this patient? Did they give Vecuronium?” And now I have to ask my dispatch, “What was the crew that was on the ground? How do I contact them when I get to the trauma center?” A lot of that stuff is alleviated with Pulsara. And we're going to go through a case in a few minutes so people can kind of see a real-world example of that.
Randy Endsley
Yeah, they might have cleared that channel, and now you have to go back and find them. But in Pulsara, you just shoot them a text and they get it, even though they're done with the call.
Corey Ricketson
Right. So, Jennifer, I know Texas had actually adopted Pulsara, and it was under state contract. So maybe you didn't have some of the regional challenges to adopt this that others across the United States have. But what was the process at the RAC level for saying, “You know what, we could use Pulsara, and let's go forward as a region”?
Jennifer Carr
We had to make a decision as a RAC—even though we didn't have all the answers, and we knew it wasn't hardwired, to just do it. This was something that we really wanted to try out, especially since it was supported by Texas, and we wanted all of our EMS in our region to be able to send the report to the ERs on any type of patient that they were bringing in. Trauma, non-trauma, didn't matter. And so we just wanted to work and get all the EMS within our 12 counties to start doing this. And that definitely took time, education, continued education, and bringing in Corey to teach them some of the tips and tricks. But we knew that there is resistance to change sometimes, especially with [the attitude of] “this is the way we've always done it,” and especially when the change is technology.
We just really had to continue pushing forward and trying this because we know some of the disadvantages of a radio report. The quality is not always good. Sometimes you miss how much Vecuronium was given. You miss that communication. Also, in some of the emergency departments that I've been in, everybody can hear that radio report, not just the people that need it. Sometimes people are hearing it that really shouldn't be hearing it. And so this was a more secure way to get good information communicated to the team in a timely fashion. We could, as Corey mentioned, send pictures and get lots of real concrete information on these patients.
Randy Endsley
Jennifer, remember, one of the things that really drew us to this was [the fact that] we've really been dealing with, how do we get our 12 leads to the hospitals? A lot of the larger services could afford the brand-new monitors that transmit. Most of the rurals could not. And so this was a fix for that, too—getting those 12 leads where they can be sent securely straight to that physician to activate a cardiac alert. So that was a big drawing force for us as well.
Jennifer Carr
We took it in steps. So basically: crawl, walk, then run. Corey likes to say that. We just had to take it in baby steps. And especially with hospital leadership, we really had to show them that this was secure. This was moving forward with technology and the benefits that we would receive in better patient care with this.
Corey Ricketson
I remember being in some of those rooms when the Coastal Bend RAC decided to just vote and go forward with this. There are always going to be some naysayers and some folks that aren't as eager to take the technology in. I just remember as a RAC, the leadership was fantastic. They said, “Look, not every question is going to be answered right now. There are going to be things that come up that we have to deal with that we don't know today, but we're willing to take that step, because guess what? Tomorrow we're going to be better than we were today. And the next day we're going to be better than that day.”
I was just looking at the calendar before this webinar. We're in November, and I remember it was right at a year ago that we started and said, “Yep, we're going to go forward with this.” It's fun to see how far we've come in that year, and we'll get into more of that.
Going back to that a little bit, Jennifer, I think a lot of people get overwhelmed with that change. And so you talked about the crawl, walk, run. Expand just a little bit on what that methodology was—to go, “Look, we're not going to try to bite off the entire cookie in one bite. So how are we going to pragmatically go about this to where we can drip a little bit of technology and expand that over time?”
Jennifer Carr
One of our biggest projects was EMS buying in—getting EMS to use technology, to use an iPhone or an iPad to communicate this report. And so we said, “Start first with your non-emergent patients that you're bringing into the ER. You know, start with those easier ones that you don't have to move so fast with, and get comfortable with that, and create the muscle memory with that.”
And then we said, “Okay, now move more with your complex patients—your more emergent patients.” And so we took time with EMS and told them, “It's okay if you're not 100% going forward with all of your medics on day one. And so we just worked with them and communicated with them monthly. We communicated at our RAC meetings, as we routed to EMS stations, asking, “How is it going?” and answering their questions. We really just took it slow with the medics.
And then we started with all of the ERs, educating the nurses and the physicians on how to answer it, what it looks like, and just kind of going slow with that and being very patient.
And also, we did not take away their backup method. We did not take away the radios. The radios are still there in the event that they ever need to use them. We did not take that away. And so I think it was comforting to them to know that the method they've been all familiar with for many years is not gone. It's still there in the event that they do need to use it.
Corey Ricketson
Awesome. Yep, for sure. And I remember too, it was, look, if we don't put a deadline out there and draw a line in the sand, then people will just not adopt. And so even though there was the approach of “Look, here's your backup, and we are going to start with the non-criticals first, there is still a drop dead date.” The RAC really pushed that to where it wasn't an opt-in, opt-out. We voted as a RAC to do it. We're going to go forward together, but we're also going to help along the way.
You touched on something, too—that this didn't just start out as a trauma initiative. That’s what we're highlighting in this particular webinar, but the decision was that we are going forward as a RAC, because this is not just for trauma. This is for all patient types, and we're going to solve the system of care problem in general. So how does the solution fit into the big picture on all systems of care?
Jennifer Carr
A lot of trauma programs—and I'm sure there's a lot on this call—are familiar with the halo effect of trauma programs. And we said, trauma will be the guinea pig. We will go first, we will figure it out, we will hardwire it, and then we'll add other service lines after that, such as STEMI, stroke, and sepsis, and we'll work towards that.
We really worked to show the halo effect of this project and that it will help improve patient care. And that's another thing when you're talking with your administration and your IT and your HR departments about this software, is making sure [they understand] that the biggest purpose of this is to improve patient care. This will improve patient outcomes. Keeping that as number one helps to get buy-in and support on this.
Corey Ricketson
Yeah. Randy, you mentioned the 12 leads as a precipitating factor for going forward with this, because people didn't have a solid plan to send in 12 leads. Well, that has nothing to do with trauma, and it may actually have nothing to do with STEMI. There are a lot of reasons that we provide 12 leads to hospitals, like electrolyte imbalances, or tachydysrhythmias, and things like that.
So being able to send better, more secure information forward prior to that patient arriving is really important—not just for trauma, but for a lot of different patient types.
Randy Endsley
Yeah, absolutely. The EKG or the 12 lead was definitely a driving force. But I'll tell you what, there's nothing that gets the trauma room ready quicker than a good picture of the incident. Your patient may sound pretty good, but here's a picture of the car that we dragged them out of. A picture is worth a thousand words, and it definitely gets things moving very quickly.
Corey Ricketson
Yeah. I was actually surprised the first week that we went live with comprehensive trauma at Shoreline. I was sitting in the ER for the week, making sure everything was going smoothly. I remember there was an ejection out of a boat there in the bay, and the boat came around and ran the individual over.
And so the medics sent pictures of eviscerated organs and a lot of different stuff, soft tissue injuries, that now that trauma team can definitely see what they need to prepare for, and perhaps even chat with that medic that's in the back of the truck on some treatment that they might consider because they're still 20 minutes away. It really moves that care way up in that cycle.
Randy Endsley
A lot of times when we get there, things are already wrapped up. They've already stopped the bleeding, they've already done their best. And so now I'm left to describe to the hospital what's under that bandage. But I'm getting second-hand information. So they can take a shot of that and then put it into our channel. Then I not only get to give a good verbal description, but then they get a visual look at it at the same time. So again, a picture is worth a thousand words. It's a great function of Pulsara.

Corey Ricketson
So, Jennifer, walk us through what a typical trauma activation was prior to Pulsara. What was your normal process?
Jennifer Carr
The radio report would be called to the ER, or maybe the patient would walk in, and they would activate the trauma team via pager. Old school pagers were used, and what came across to the team that was carrying the pagers was just basically a bunch of numbers—911 if it was a level one activation, and 922 if it was a level two activation. And that's it. They didn't get any information on what room the patient was going to, what the ETA was, or any information about the patient.
And so the next step forward that we took with Pulsara was not only receiving the reports from EMS, but then turning around and taking that information, that exact report we received, hitting “activate,” choosing the trauma activation level, and then it would go to the trauma team with all of that information.
Corey Ricketson
This was fascinating to me when we went live, and I was in the ER, and we had our first trauma activation. Of course, we were running dual process, so the ED clerk called the PBX operator. They sent out the pages, and then the Pulsara alert was sent at the exact same time. And the trauma team and trauma surgeons were actually in the room with the patient doing their assessment. And I want to say it was like 5 minutes later or something that Dr. Adamski’s pager actually went off and he looked at it and said, “Oh, I'm being told there's a trauma activation,” when he's already got his hands in the patient. So those delays [with antiquated technology] are definitely sometimes quite significant.
As you describe now, basically, what happens is when that alert is sent, the ED starts to look at the information that was presented. And, you know, sometimes they are looking for that nugget that can tell them, I need to move this patient to a level one activation versus a level two.
And so they're consuming things like vital signs or pictures of injuries, [which helps them decide whether to] select level one or level two. They press this big orange Activate button, and then there's a preassembled team of individuals that are on call to receive those alerts. In the example below, blood bank, anesthesiologist, pharmacy, and trauma surgeons are all included in the group.

In this image, I can see that three of the people on my trauma team have actually seen this. You can even dive in even further and look at specific individuals. There are logs around this. Accountability is certainly something that you see with this.
Let’s say I'm a trauma surgeon, and I was brought into this channel. You can see there are two images for this patient. They can look at those and start to consume a lot of the information. This also can go to registration at the same time, so these patients can get pre-registered and just start that process even faster.
Jennifer Carr
A lot of hospitals do overhead paging, and so this has been able to take that away. The overhead paging is distracting to patients and families that are trying to heal. Also, overhead paging sometimes brings the looky-loos down to the department because they want to see what's going on when they've just heard five traumas paged in the last 30 minutes. This software has helped to fix that issue too.
So just like I talked earlier about the crawl, walk, run—we did that not only with the prehospital, we did it with the hospital for this activation process. We started first with our trauma program team and our trauma surgeons. We got everybody access. We let them keep their pagers, so we have a duplicate process on this until they're comfortable with it. But we started with the trauma surgeons first on receiving this and getting comfortable with that, and then we added in pharmacy. We added in security.
And so we basically kind of took it two weeks at a time, where we added in a new group of people, we got them access, we did education training with them, and we just kind of continued to grow each department that responds to a trauma activation to add them in. And then there's turnover in some departments, and we have to go back and do more continuing education with them.
Then there were some departments, such as maybe the O.R. board runner, or maybe PBX, that don't need a handheld device. So we got them set up on a web browser so that they can receive these activations and notifications that way. And so that helped some of the departments that maybe did not have hospital-issued handheld devices to be able to use that option to receive these notifications.
Corey Ricketson
Yeah, that's a great point that you don't have to have a mobile device. I think a lot of the people that utilize Pulsara are mobile, so that opportunity is a huge advantage. You know, I'm on call, but I'm off-site, and so now I've got this mobile device. But if I'm in a seat and I've got computers in front of me, and that is what I do all day, such as registration, ED clerks, or PBX operators, then I can use the browser. It alerts me and everything, just like a mobile device. So that flexibility is definitely good.
One of the things I noticed, too, to give Jennifer some accolades, is that staying on this process from an executive sponsor standpoint is so important. I could not implement this without that type of leadership. And for Jennifer to stay on those groups and say, “Hey, PBX group, this is Corey. He is going to set you up; I'm going to follow along and make sure that you don't need anything else.” And then along the way, if we notice that there are hiccups, going back and re-addressing that with reeducation or perhaps a different type of device. It's all of those types of things. But instead of just saying, “Okay, Corey, go implement this, and I'm out of here,” it was really, “I'm right there with you, and I'm going to help this process.” From an executive sponsor standpoint, that's a huge key to success.
Check out Part 2, in which Jennifer, Randy, and Corey discuss more workflows and how they're scanning the Texas statewide wristbands for better patient tracking!
What does it take to build a system of care that scales? Eric Epley, Executive Director of the Southwest Texas Regional Advisory Council (STRAC), and Corey Ricketson, Pulsara's Sales VP - Texas, discuss the benefits of using the same communication platform for everyday patient transports, transfers, and transitions of care and stress events. Watch the webinar here!

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...