Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
11 min read
 Team Pulsara
:
Sep 20, 2021
Team Pulsara
:
Sep 20, 2021

Editor's Update: The ET3 program is mentioned throughout the below report. Please note that, as reported by JEMS.com on 6/28/23, the federal government is ending the ET3 program. According to the Centers for Medicare & Medicaid Services, “This decision does not affect Model Participants’ participation in the Model through December 31, 2023.” Read the full article on JEMS for more details: ET3 Program Comes to an Abrupt End. Be advised that Mobile Integrated Healthcare and Community Paramedicine are separate initiatives and are unaffected by the ET3 program termination.
Editor's Note: On August 11th, EMS1, Fitch & Associates, and the National EMS Management Association released their fourth annual EMS Trend Report, proudly sponsored by Pulsara. Because the articles and advice found within contain such critical subject matter, we've elected to publish each segment one at a time here on our blog. Read, enjoy, share, and take to heart the following information brought to you by the most prestigious thought leaders in EMS. Today's entry is a roundtable discussion with a panel of distinguished industry experts, conducted by Kerri Hatt, Editor-in-Chief for EMS1.
The COVID-19 pandemic forced EMS providers, leaders and educators to shift gears, in service delivery, in training and in where EMS fits into public health. While the biggest challenges in EMS are not new – retention, burnout, salary, mental health – the ever-evolving public health emergency shed new light into how staffing, safety and sacrifice influence provider optimism and wellness.
The sixth annual EMS Trend Report explores how the last year has shaped EMS resilience. We asked industry experts to analyze how the results reflect current healthcare trends, what they mean for the future of EMS service delivery, and how they can guide efforts to support providers in the years ahead.
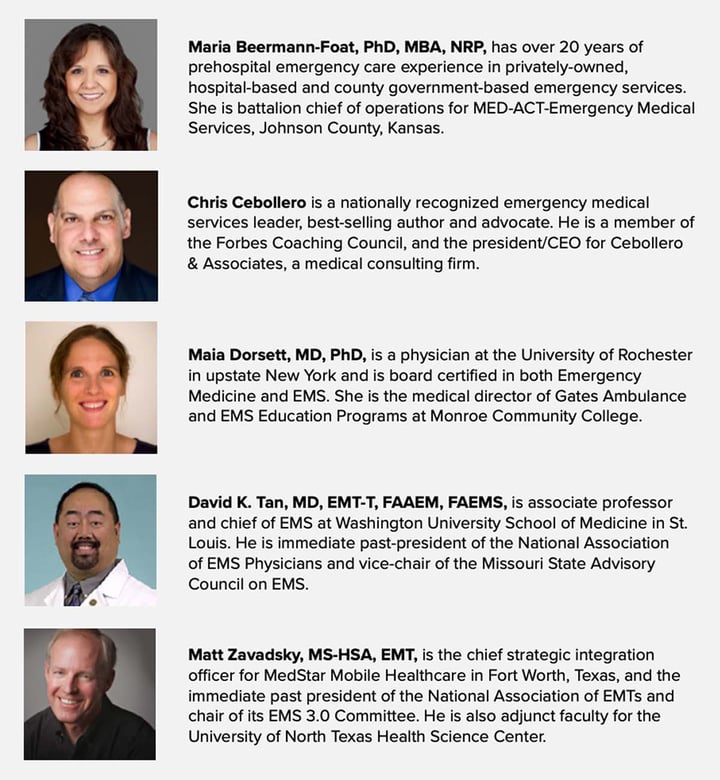
The panel includes:
Beermann-Foat: I was surprised to see that the percentages for level of burnout categories were relatively constant to the 2020 results. While a quarter of the respondents said they had one or more symptoms of burnout, almost as many responded that they have no symptoms of burnout. Also, 39% of respondents acknowledged that though they may have less energy and more stress, they did not feel burned out. Together, 63% of respondents denied having burnout symptoms.
When I speak with other industry leaders, they often relay sentiments that personnel seem to be more pessimistic, disgruntled, apt to resign, or in school to become an RN to get out of EMS. This seems counter to what this data shows and makes me wonder if these perceived anecdotal negative characterizations are actually indicating engaged employees?
I frequently tell others that engaged employees complain about the things that bother them, because they care about their work and the organization they work for, while apathetic employees remain silent.
Cebollero: A couple clinical findings raised an eyebrow for me. Seventy-five percent of respondents stated they are able to terminate arrests in the field. I would have thought this number would have been higher. Next, 58% stated they use some kind of mechanical CPR device, this was higher than I would have expected.
Dorsett: Given how the pandemic has impacted so much in our lives and in healthcare, what I found the most surprising was how little change there has been between last year’s pre-pandemic survey results and this year’s. Some areas have come into greater focus amidst these challenges, such as provider mental health, provider safety, education of the workforce and a need for improved leadership. However, many components, such as optimism about the profession, recommending the career to the younger generations and rates of burnout remained stable. This highlights a resilience in our people and systems, and reminds us that most changes remain incremental, despite transformative events.
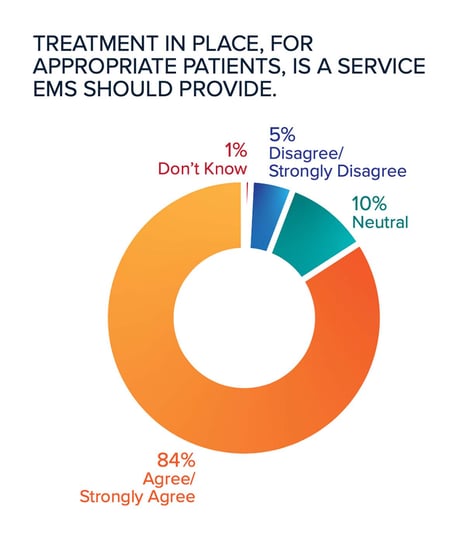
Tan: I was pleasantly surprised at the degree of support (84%) for treatment-in-place (TIP) programs beyond the pandemic emergency declaration. This gives me great hope that the vast majority of respondents truly see themselves as the healthcare clinicians that they are.
Zavadsky: Once again this year, the issue of recruitment and retention of quality personnel, and caring for the mental health of our workforce ranked as some of the top concerns for the respondents. This is both surprising and not surprising at the same time. The pandemic took a significant toll on an already beleaguered EMS workforce. Sadly, many EMS practitioners contracted the COVID-19 virus, and far too many succumbed to the illness. This led to appropriate fears of contracting COVID-19, which led many EMS practitioners to leave the profession, or seek careers in settings that may be perceived as safer than the unpredictable EMS environment, such as hospitals or other medical settings.
The plight of rural EMS agencies closing due to lack of staff has also been highlighted. EMS leaders, and the communities we serve, need to get serious about EMS workforce issues before it’s too late! Many national EMS associations, like the National Association of Emergency Medical Technicians, the American Ambulance Association, the International Association of Fire Chiefs, and the International Association of Fire Fighters are working collaboratively on EMS workforce issues, recruitment and retention, as well as practitioner stress and burnout. EMS practitioners are held in very high esteem, especially as a result of the pandemic, but those willing to enter, or stay in the profession are dwindling. Finding the right solutions will take continued collaboration, educational innovation, and will require system leaders, including medical directors and regulators, to take a hard look at things like the concepts of all ALS systems, EMT scope of practice, EMS educational standards that may be a barrier to course availability and a sincere commitment to practitioner health and well-being.

Beermann-Foat: This increasingly complex pandemic environment brought to light EMS weaknesses and inefficiencies, but also a wider realization of EMS being an essential service that is often taken for granted by the communities we serve. The challenges, from obtaining PPE, to supply chain breakdowns, a shift to online learning and adapted service delivery models, may shift our industry focus toward improving individual provider’s well-being, while continuing to advance how we provide EMS services, more so than in previous years. For example, mental health has been a topic in recent years and efforts have been started to address provider mental resiliency, however, many of us took for granted that we had provider safety fairly well managed. We’ve come to realize that planning for safety and ensuring safety can be very different animals, especially in the environment we have encountered over the past 18 months. Many news stories across the nation spotlighted just how fragile our safety systems are. Available and upcoming technology has the potential to help EMS agencies balance provider safety and well-being while still delivering needed services.
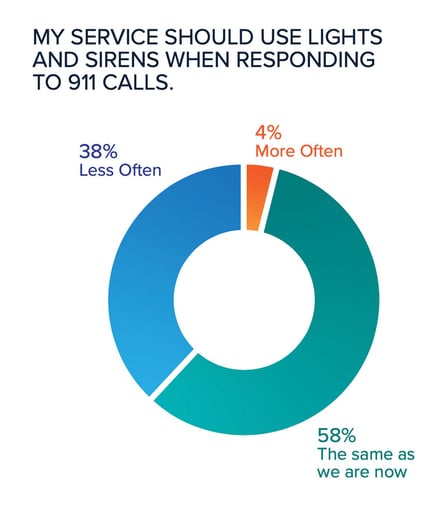
Dorsett: In response to the pandemic, all areas of healthcare had an increased focus on provider safety and mental health. I hope even as we move forward from the pandemic, we capitalize on this safety focus by addressing daily threats to the safety of our clinicians: lights and sirens use, clinician mental health and fatigue. There is both hope and work to do here. While the percentage of “very often” response with lights and sirens actually went up, 38% responded that lights and sirens should be used less often.
Tan: Respondents in 2021 clearly felt like clinician mental health became a higher priority for their employers, and I think this was largely due to the much higher awareness of this issue during the pandemic response efforts of 2020. This aligns across the healthcare industry, where frontline health workers were recognized as the ones bearing the most stress, both at home and in the workplace, at the peak of the battle against COVID-19.
We must not let the momentum of support for EMS wellness wane simply because the infection rate decreases and the sense of urgency begins to lessen, as the everyday stressors of prehospital care are still present, only to be augmented when the next infectious disease threat strikes. Permanent solutions to better mental health support, response, and resilience should become more routine for EMS services as we benefit from lessons learned during the pandemic.
Zavadsky: The Trend Report identified that EMS roles such as treatment in place and transport
to alternate destinations are viewed as a key to the future of EMS. The implementation of the CMS Emergency Triage, Treatment and Transport Model (ET3) has not only mainstreamed these roles, but has also generated additional interest in this model by other payers. Several states, including Texas, recently passed legislation to facilitate Medicaid payments for similar models. Further, Medicare waivers during the public health emergency for transport to alternate destinations, and payment for non-transports of patients if part of a community-wide EMS protocol are further examples of the value
CMS places on these expanded EMS roles. Although admittedly, these waivers have had little practical impact, the fact that they have been issued has served as a platform for national EMS associations to engage with legislative and regulatory stakeholders to expand these models beyond the public health emergency.

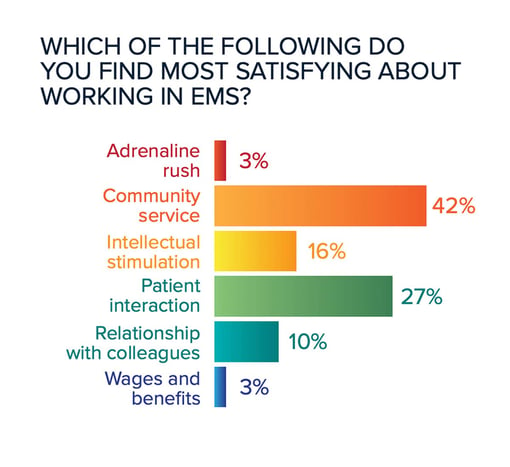
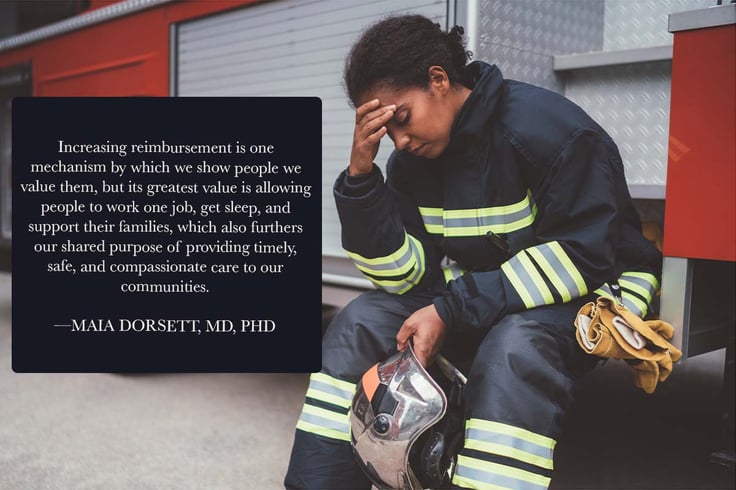
Beermann-Foat: Wages and benefits are again at the bottom of the satisfaction scale ratings and 45% of respondents either disagreed or strongly disagreed that their organization was doing enough to address clinician fatigue. Fifty-nine percent of respondents stated that their agency struggles to recruit quality candidates, while 56% stated poor leadership is either a significant or major issue. Each of these are contributing factors in employee retention, with at least three of the four being within an organization’s leadership domain. Of course, wages and benefits will be a continual struggle for EMS until our reimbursement model is modified to allow for greater revenue. I would encourage EMS providers and leaders to continue or become involved in national efforts to get the federal government to change CMS/ reimbursement rules.
Clinician fatigue mitigation efforts are dependent on the EMS system’s model but can be incorporated with enough creativity or flexibility to current practices. For example, one EMS agency in the Kansas City area has implemented a “fatigue trigger” notification to field supervisors when a crew reaches a pre-identified UHU threshold within a rolling 5-hour block of time. This allows field supervisors to make real-time contact with the crew to check on their perceived fatigue status and allow for a short break should the crew feel a break would be beneficial. This same agency combats crew fatigue by staffing additional units during high-demand periods identified through CAD modeling of previous years’ data. Agency leaders should examine their staffing models and workload requirements to discover simple changes to help mitigate personnel fatigue.
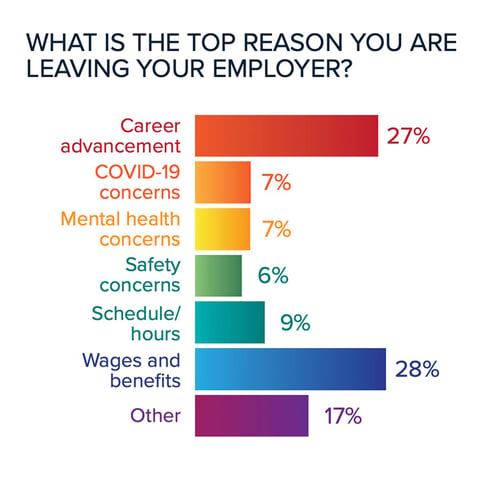
Cebollero: Retention is again the No. 1 answer as to challenges inside EMS agencies. This is not surprising, as retention has been a big challenge for decades. The old question “Is EMS a career field or a steppingstone?” comes to mind. Looking at the response as to why people are leaving EMS positions, career advancement is No. 1 and pay and benefits are No. 2. Until we can address the career progression and pay issues, I am not sure we can get EMS providers to stay in the field, especially if there are no positions that will allow EMS providers to promote for career advancement. EMS agencies must create leadership development programs to assist providers in understanding the science of leadership, and assist their search for next-level EMS positions.
Dorsett: The survey results indicate that EMS is made up of individuals who believe in a just cause bigger than themselves, but who do not feel valued or supported by leadership in doing so. Consider the following points:
Wages and benefits are but one expression of value. It is easier to blame extrinsic factors than to address bigger issues, such as trust and support, which take effort to build but are harder to dismantle once established.
Tan: Time and again, the EMS Trend Report has revealed an impression that EMS leaders over-emphasize recruitment without addressing meaningful retention efforts. By retention, respondents consistently rank low pay and a lack of upward mobility opportunities for career advancement as key reasons for abandonment of EMS as a career choice. In fact, many have gone so far as to say EMS cannot be considered as a career but as a mere steppingstone to nursing school, the fire service or hospital-based jobs. Thus, if EMS is ever to be viewed as a serious career choice in and of itself, then as an industry, we need to begin focusing on retention efforts that include better compensation that is linked to advanced education and requisite opportunities for advancement. This includes getting payers
to view EMS as an integral part of the healthcare system as opposed to being viewed as “only a transport service” to healthcare.
Zavadsky: EMS leaders, regulators and local communities need to realize that the provision of EMS is an essential public service, and fund it as such. Thankfully, several states have made EMS an essential service, creating a funding mechanism that allows EMS agencies to address the pay and benefit challenges for EMS systems. While this is welcome activity, it is now incumbent on the EMS agencies to continually prove value to those who are paying for EMS services. We need to be more than simply a method of conveyance to an emergency department. Taxpayers and other payers should understand the enhanced roles more and more EMS agencies are undertaking to support the healthcare system, and the community. These enhanced roles can, and should be, partnerships with public health for virus testing, immunization and treatments of patients who contract viruses; and being part of the out-of-hospital healthcare system through programs like the “Hospital at Home” model and the facilitation of telemedicine for patient treatment and navigation during 911 responses.
Beermann-Foat: The data supports the idea that a majority of current EMS providers still have
a passion for prehospital medicine despite its shortcomings. Survey respondents again listed retirement as the primary reason for leaving EMS, with continuing employment with another EMS agency as the second reason. This is promising because it supports current providers want to continue working in EMS as long as possible. However, there was a small uptick in the percentage of respondents who identified they plan to leave EMS for other healthcare employment.
I believe that EMS is at the beginning of an industry evolution. While the pandemic certainly brought about acknowledgement of major pitfalls in doing what we do, it also brought about a great deal of positive realizations. The general public became significantly more aware of EMS and other healthcare providers as essential services. Many EMS agencies also realized how closely EMS and public health departments can collaborate to meet citizen needs. EMS providers were challenged with learning new equipment, using different types of PPE, becoming more diligent with unit/equipment sanitation procedures, and advocating for patient needs in the midst of obstacles outside of their control. But, most importantly, the federal government opened the door for change of reimbursement models. Having tenured EMS providers involved in discussions concerning these important topics can help move the needle forward even further.
Cebollero: In 2020, many thought mobile integrated healthcare was the future of EMS, and I agreed. What surprised me this year was the low percentage of those who think telemedicine is the future of EMS. In the days of MIH and ET3, and on the heels of COVID-19, telemedicine is in fact the future of how we will be able to conduct our business more effectively. As a matter of fact, during the pandemic, we moved most of our MIH visits to an online platform with great success. Future models may include a hybrid of home visits and telehealth components.
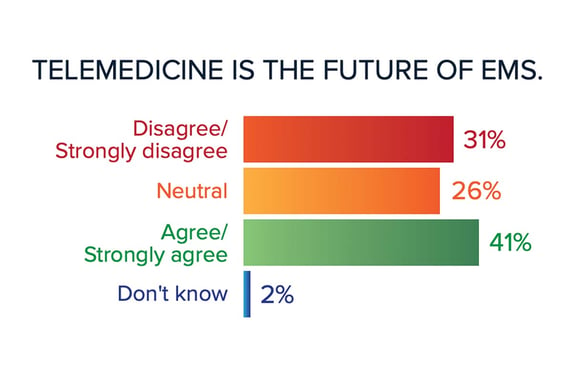 Dorsett: The future direction of EMS is to evolve in how we care for our communities. The data in this survey suggests that EMS clinicians are ready to be engaged in such endeavors. EMS clinicians find more satisfaction in community service and patient care than in the adrenaline rush of a critical call. Overwhelmingly, 84% of respondents felt that treatment in place, for appropriate patients, is a service that EMS should provide.
Dorsett: The future direction of EMS is to evolve in how we care for our communities. The data in this survey suggests that EMS clinicians are ready to be engaged in such endeavors. EMS clinicians find more satisfaction in community service and patient care than in the adrenaline rush of a critical call. Overwhelmingly, 84% of respondents felt that treatment in place, for appropriate patients, is a service that EMS should provide.
The role of leaders is not only to advocate for the redesign of the system to enable this evolution, but to prepare EMS clinicians for these expanded roles.
Regarding advocacy, this expands beyond reimbursement models (which are already actively changing with initiatives such as ET3), to the recognition of EMS as healthcare professionals by the public. Indeed, 86% of survey respondents felt that their organization did not effectively educate the public about what EMS professionals do.
Regarding preparation of the EMS clinician, educational curricula and continuing education efforts need to be expanded with focus not just on chronic health conditions, but on social determinants of health, quality improvement efforts and issues of healthcare navigation. We need to make sure that the primary motivator for non-transport remains matching resource to patient need and improved health outcomes, rather than decreasing resource utilization alone.

Tan: In spite of the many concerns respondents brought forth in this year’s Trend Report, there were many positive things to note, including the persistent optimism for EMS in the face of many industry challenges. People seem to choose prehospital medical practice because they genuinely enjoy meeting the needs of others, contributing to the communities in which they live, and getting a chance to make a difference in peoples’ moments of crisis or need. Thus, the future direction of EMS is one of adaptability and growth to include what I think will be a redefinition of EMS medicine as MIH, ET3 and TIP programs become standard activities of EMS services across the nation.
Zavadsky: The good news? EMS is proving our value in ways far beyond a simple 911 response and subsequent transport to an emergency department; and a value that payers are becoming more willing to pay for. This may open the door to a more sustainable economic model for EMS in the future. However, the immediate crisis of the shrinking EMS workforce and the immediate financial crisis for EMS agencies, especially in rural communities, may lead to more EMS agency closures. EMS leaders and national associations must continue to find both immediate and long-term solutions to the EMS conundrum – enhanced value through enhanced roles, but the slow adoption of payers, including taxpayers, to pay for those services.
Pulsara is helping with COVID-19 management by helping mitigate patient surge, streamlining patient transfers, minimizing exposure, and more. Learn more about COVID-19 + Pulsara here.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...