Pulsara Around the World - February 2026
January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...
3 min read
 Team Pulsara
:
Apr 12, 2019
Team Pulsara
:
Apr 12, 2019
EDITOR'S NOTE: Special thanks to Courtney Chumley, FACPE, for writing today's blog post. You can connect with her on LinkedIn.
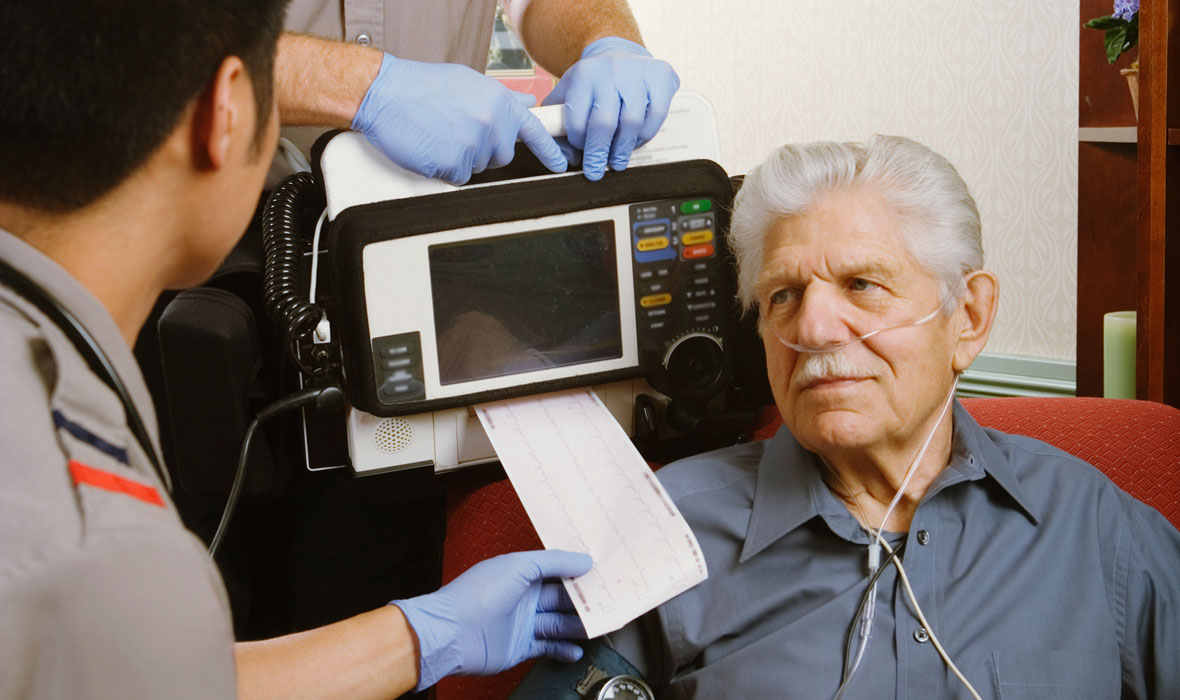
Every first responder has gone through EMT and/or Paramedic school and remembers the very short section that covered how to explain to a family that their loved one has died. “Don’t use vague words. Make sure you use 'has died' and 'is dead.'” But after 20 years of field experience, that section did not equip us with nearly enough information to help these family members cope far into the future.
Throughout my career, I have spoken with many people who have suffered a sudden loss. I have heard the same information from them: they didn’t know what was going on. No one was talking to them and letting them be a part of the process. The family and bystanders wonder if they could have done more to help. Then, they wonder what happens next.
There was a turning point in my career 12 years ago where I was on-scene at an unexpected cardiac arrest in a 28-year-old male. He had the flu for a few days and collapsed in front of his young wife. We were doing our best to resuscitate him, when I heard his wife ask “I don’t know if any of you believe in God but can someone please pray with him real quick?” Before I could say a word back, someone else on scene replied “we don’t have time for that right now.” To this day, I am still bothered by that momentary lack of compassion. All that was requested of us was to say a few silent words to him on behalf of her beliefs to help bring just a moment of comfort and hope to a terrifying situation.
Family members deserve to have benevolent providers who are able to break from the script and show a few drops of humanity during their greatest times of need. I have become more compassionate throughout my career after seeing countless lives destroyed in an instant. I make sure to follow up with the young life guard who, at age sixteen, did CPR on a two-year-old. We know that the child will not survive, but we tell him he did an amazing job and he gave the child his best chance at survival. I have learned that no amount of training prepares a 16-year-old for those feelings of guilt and helplessness.
I have asked the 80-year-old husband if he wants to tell his wife he loves her one last time before we transport her into the truck, and I've had the medic crew pause for a few seconds so he can have that moment. Too many times we have all heard “I didn’t get to say goodbye.”
My three children lost their Dad at a young age, and even with all of my training and experience witnessing this kind of scenario, I felt so lost. That's why it meant the world when a fellow first responder came to my house and dropped off a letter with information for the social security office, child grief counseling groups, and numbers to places I would need to contact in the coming days. I find myself repeating this act of kindness when I visit scenes where this information could be supportive.
How much information do we tell the family while we are coding their loved ones? While every situation is different, I've found the best results in telling them that their loved one is in critical condition, that their heart is not beating, that they are not breathing on their own, and that we are doing everything we can. I want the family to know how grave the situation is -- I try to give them an opportunity to say goodbye before we leave.
We are BUSY on these scenes. I know. I still work them. We are desperately fighting against something greater than ourselves to save our patients. Not every agency has enough people on scene to allow this communication with family members in those early moments, but if you take anything away from this post, try to find a moment to reach out to the family, be compassionate, be informative, and tell them you are grateful for any assistance they provided before you got there. Those families are watching everything we do without understanding why. You are the beginning of a horribly painful journey for the family, but you can help shape that journey with communication and compassion.

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...

At Pulsara, it's our privilege to help serve the people who serve people, and we're always excited to see what they're up to. From large-scale...