Pulsara Around the World - March 2026
February Recap From neuroscience symposiums to EMS expos, our teams traveled to five shows in February. Our events schedule is slowing down in March....
1 min read
 Max Landon
:
Nov 25, 2025
Max Landon
:
Nov 25, 2025

The quality improvement project from CommonSpirit Mercy Hospital in Durango, Colorado, demonstrates how streamlined communication and standardized field activation—powered in part by the Pulsara platform—can significantly reduce STEMI treatment times in rural settings.
The rural mountain hospital had long faced challenges common to remote regions: long transport distances, unpredictable weather, limited local resources, and no prehospital STEMI activation process. In 2024, 60% of their first medical contact–to-device (FMC-to-device) times exceeded the guideline-recommended 90-minute threshold, averaging 111 minutes.
To address this, the hospital launched a multidisciplinary, multiagency improvement initiative involving ED clinicians, interventional cardiologists, cath lab teams, EMS physician directors, and five regional EMS agencies. A key component of the project was implementing the Pulsara communication platform to support early STEMI recognition and real-time team activation.
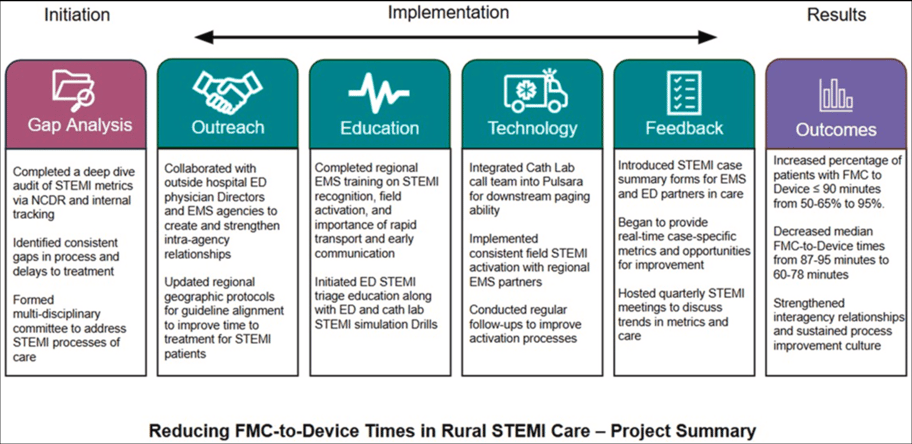
With Pulsara, EMS could transmit ECGs and patient information in real-time, allowing ED physicians and interventional cardiologists to review cases within two minutes and activate the cath lab directly from the platform.
After launching the new processes in February 2025, the hospital saw dramatic improvements:
These gains demonstrate that even in geographically challenging regions, coordinated communication and streamlined activation can eliminate avoidable delays and save more heart muscle.
Rural hospitals often face barriers that make guideline-directed STEMI timelines feel out of reach. This published research study shows that with authentic collaboration, standardized processes, and real-time communication technology, rural teams can meaningfully improve outcomes even in the most challenging environments.
To learn more about how CommonSpirit Mercy Hospital is transforming rural STEMI care with Pulsara, check out this AHA podcast interview with CommonSpirit Mercy CEO, Josh Neff.

February Recap From neuroscience symposiums to EMS expos, our teams traveled to five shows in February. Our events schedule is slowing down in March....

January Recap The start of 2026 was on the slow side for our events schedule, with our team heading to the Florida Fire & EMS Conference, the...

Recent research shows how Pulsara was successfully leveraged to connect more than 6,000 COVID-19 patients to monoclonal antibody infusion centers via...