COVID-19 Management
Teller County is a rural community in Colorado with a population of just over 25,000 people. Ute Pass Regional Health Service District provides ambulance service to 539 square miles of mostly mountainous terrain in portions of four separate counties: Teller, El Paso, Park, and Douglas. Most of the area they cover is extremely rural, and transport times range anywhere from five minutes up to multiple hours.
In addition to long transport times, patients feared going to the hospital in the midst of a pandemic; therefore, many in the community were not receiving the care they needed—until clinical leaders launched a 911-initiated telemedicine program.

As EMS and hospital leaders in Teller County, Colorado watched cities like New York grapple with COVID-19 in March of 2020, they knew they needed to carefully plan their response. Fear of the virus spread even faster than the virus itself, and it quickly became apparent that nearly half of Teller County’s residents were reluctant to seek care—for any condition—at the hospital.
Dr. Jeremy DeWall, EMS Medical Director for the Teller region, observed the trend firsthand. “Up to 40% of our EMS volume does not want to go to the hospital once 911 arrives,” he said. “Looking at our numbers, the fear was that we were missing a large group of people who were without healthcare or afraid to go to healthcare because of COVID-19.”
COVID-19 Management
Reaching Underserved Populations
Connecting patients and paramedics with a physician via telehealth
Teller County has a robust and successful community paramedicine program and were already using Pulsara, a healthcare communication and telehealth platform, for EMS and hospital communication when COVID-19 hit. Their paramedics were accustomed to securely sharing patient information and communicating with the hospital through the Pulsara platform. That gave James McLaughlin, Director of Community Paramedicine at Ute Pass Regional Health Service District, an idea. “Community paramedics are in the field. We’re mobile. We’re used to going into people’s homes, and it’s relatively safe for us to do so. There aren’t as many physicians as there are community paramedics. We’re able to go from call to call, while the physician sits in one location and teams up with community paramedics to provide their services.”
With that concept in mind, McLaughlin joined forces with Dr. DeWall and Emergency Medical Specialists, PC, a group of board-certified emergency medicine physicians serving as ED physicians throughout the region, to set in motion a 911-initiated telemedicine program.
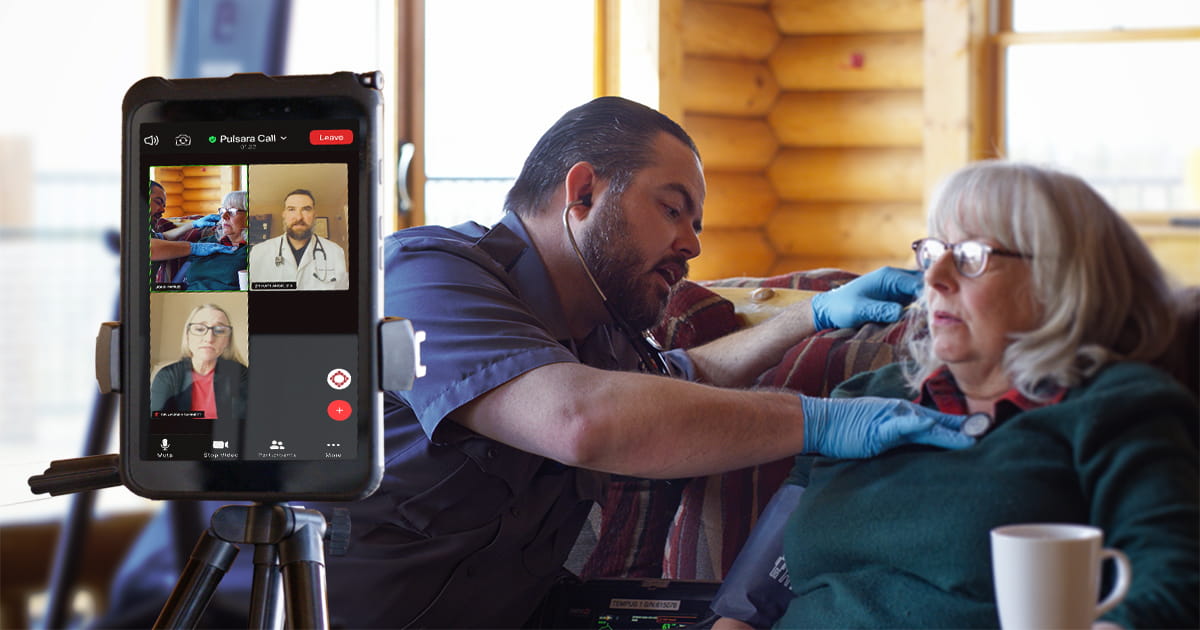
As Teller County’s community paramedics respond to each call, they ask patients whether they want to be transported to the hospital. If they don’t and are clinically safe to remain at home, paramedics run a full assessment. Using Pulsara, they create a new patient channel and upload the patient’s vital information. Medics can take pictures of the patient and of the tests they perform, and upload them into Pulsara. A medic may then use Pulsara to contact a board-certified emergency medicine physician for telehealth. These physicians are on call for telehealth visits only.
Once the physician has viewed the patient information in Pulsara, they initiate a live video call with the medic. The doctor can then see and speak with the patient, working with the medic in real time to diagnose and treat the patient. “Not to say that my assessment isn’t important,” said McLaughlin, “but there is something about bringing a physician in and their ability to provide additional services that we can’t that really completes that circle. And being able to do that anywhere is such a powerful tool for agencies like ours.”



While the program is still in its early stages, Teller County has already seen some promising results. They’ve successfully reduced the number of possible exposures to COVID-19 by avoiding transport to the hospital when possible, while also meeting patients in an environment they’re comfortable with. In addition, patients who didn’t want to go to the hospital and otherwise would not have received an evaluation and care by a board-certified emergency medicine physician have received care in their home, including medications, referrals to primary and specialty physicians, and other community resources. The community paramedics have also worked with patients on fall risk assessments and management, referral to mental health and substance use disorder providers, and engagement with the senior coalitions.
The program has been very well received by patients—particularly Teller County’s older residents. “The biggest embracers of this so far have been our geriatric population,” said McLaughlin. “They love this because they know they’re at risk by leaving the house. And because this technology is so seamless for them, they embraced it wholeheartedly. We have them grabbing the tablet from us, saying, ‘Son, just get out of my way. Let me talk to the doc.’ It’s fantastic. It’s incredible how it’s increased their access to services.”

According to Dr. DeWall, the program has helped reach patients who would not otherwise have received care. “We’re seeing this pilot program actually helping that vulnerable population of people who are afraid or unwilling to go to the hospital, and getting them connected with long-term resources, or at least getting them through their acute situation. It’s worked very well.” This same team is now working with multiple other agencies in Teller, Park, and El Paso Counties to expand the pilot program. They have received support from the Newmont Cripple Creek Victor Gold Mine and Lieutenant Governor’s Office, through grants, to help support this pilot expansion.